ICA/CCA Ratio: What Your Results Really Mean & What's Next
Understanding the ica/cca ratio is crucial for assessing the viability of various business ventures. Specifically, financial institutions often leverage this metric, comparing it against established industry benchmarks. A deeper understanding of the Internal Capital Adequacy Assessment Process (ICAAP) requires careful calculation and interpretation of the ica/cca ratio, as it directly influences capital allocation strategies. Furthermore, regulators like the Federal Reserve closely monitor these ratios to ensure financial stability and mitigate systemic risk, assessing the efficacy of a firm's Capital Contingency Plan through it. The ica/cca ratio, therefore, offers a vital lens through which to evaluate the overall health and resilience of an organization.

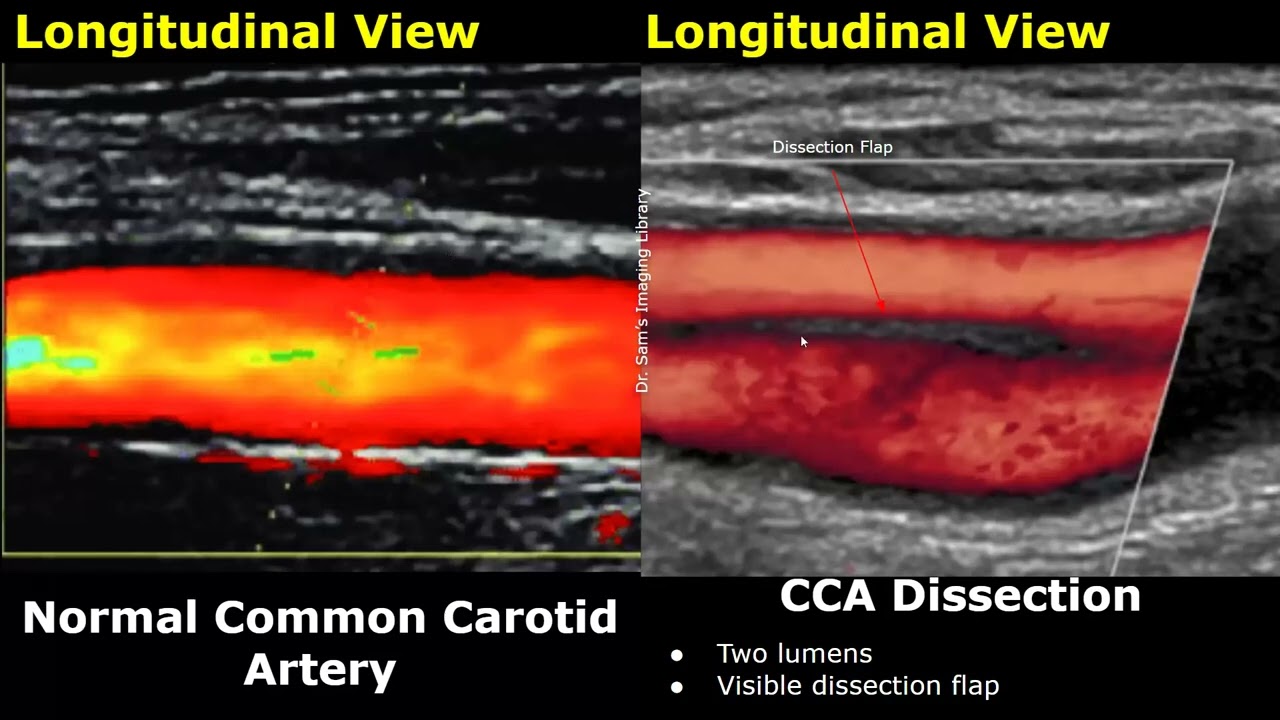
Image taken from the YouTube channel Medmastery , from the video titled Distinguishing the ICA from the ECA with ultrasound .
The Internal Carotid Artery/Common Carotid Artery (ICA/CCA) ratio is a critical metric used in the non-invasive assessment of carotid artery stenosis, a narrowing of the carotid arteries in the neck. These arteries are the primary blood suppliers to the brain, and any significant obstruction can dramatically increase the risk of stroke. Understanding this ratio is key to interpreting the results of carotid ultrasound examinations and making informed decisions about vascular health.
Defining the ICA/CCA Ratio
The ICA/CCA ratio is, in essence, a comparative measure of blood flow velocity. It is calculated by dividing the peak systolic velocity (PSV) in the Internal Carotid Artery (ICA) by the PSV in the Common Carotid Artery (CCA).
This ratio provides valuable insight into the hemodynamics of blood flow in the carotid arteries.
A higher ratio suggests that blood is flowing faster through the ICA relative to the CCA.
This difference in velocity often indicates a narrowing or stenosis in the ICA.
The increased velocity is the body's attempt to maintain adequate blood flow to the brain past the point of obstruction.
The Ratio's Role in Detecting Carotid Stenosis
The ICA/CCA ratio is a cornerstone in the diagnostic process for carotid stenosis. Carotid stenosis is often asymptomatic until a significant event, like a stroke or TIA, occurs.
Therefore, early detection via screening and diagnostic ultrasound is crucial.
The ICA/CCA ratio, when interpreted in conjunction with other ultrasound findings, can help identify even subtle degrees of stenosis. It helps guide further investigations and potential interventions.
Elevated ratios raise a red flag, prompting clinicians to consider further diagnostic testing and risk stratification.
Demystifying Results and Guiding Next Steps
This article serves as a guide to demystify the often-confusing results of ICA/CCA ratio measurements. Our aim is to empower you with the knowledge to understand your carotid ultrasound report and participate actively in discussions with your healthcare providers.
We aim to translate the technical jargon into clear, understandable language.
We will outline the significance of different ratio values.
We will also provide a framework for understanding the potential next steps in diagnosis and management.
Our goal is to provide clarity and direction, ensuring you are well-informed and proactive in managing your vascular health.
The ICA/CCA ratio is a cornerstone in the diagnostic process for carotid stenosis. Carotid stenosis is often asymptomatic until a significant event, like a stroke or TIA, occurs. Therefore, early detection via screening and diagnostic ultrasound is crucial. Now, let's delve into the specific arteries involved and how the measurements are obtained, clarifying the basis for understanding the ICA/CCA ratio.
The ICA and CCA: A Basic Anatomy Lesson
To fully grasp the significance of the ICA/CCA ratio, it’s essential to understand the anatomy of the carotid arteries and how blood flow within them is measured. The Internal Carotid Artery (ICA) and the Common Carotid Artery (CCA) play critical roles in supplying blood to the brain.
Defining the Internal Carotid Artery (ICA)
The Internal Carotid Artery (ICA) is one of the two main branches of the Common Carotid Artery.
It is responsible for delivering oxygen-rich blood to the anterior (front) portion of the brain, as well as the eyes.
The ICA branches off from the CCA in the neck and ascends into the skull, where it further divides into smaller arteries that supply the cerebral hemispheres.
The health of the ICA is paramount for maintaining cognitive function and preventing stroke.
Understanding the Common Carotid Artery (CCA)
The Common Carotid Artery (CCA) originates from the aorta (on the left side of the body) and the brachiocephalic trunk (on the right side).
It ascends through the neck and bifurcates (splits) into two main branches: the Internal Carotid Artery (ICA) and the External Carotid Artery (ECA).
The CCA serves as the trunk that feeds both the Internal and External Carotid Arteries.
It provides blood flow to the face, scalp, and other structures in the head and neck via the ECA.
How Duplex Ultrasound Measures Blood Flow Velocity
Duplex ultrasound is a non-invasive imaging technique used to assess the structure and function of blood vessels.
It combines traditional ultrasound, which produces images of the arteries, with Doppler ultrasound, which measures the velocity of blood flow.
During a carotid ultrasound, a transducer is placed on the neck to emit sound waves that bounce off the blood cells moving through the arteries.
The Doppler component of the ultrasound measures the frequency shift of these sound waves, which is directly proportional to the velocity of blood flow.
This allows clinicians to determine the peak systolic velocity (PSV) in both the ICA and CCA.
Calculating the ICA/CCA Ratio
The ICA/CCA ratio is calculated by dividing the Peak Systolic Velocity (PSV) in the Internal Carotid Artery (ICA) by the PSV in the Common Carotid Artery (CCA).
Formula: ICA/CCA Ratio = ICA PSV / CCA PSV
For example, if the ICA PSV is 150 cm/s and the CCA PSV is 50 cm/s, the ICA/CCA ratio would be 3.0.
This simple calculation provides a valuable indication of the relative blood flow velocities in these two critical arteries.
Interpreting the Ratio: What It Represents
The ICA/CCA ratio essentially reflects the comparative speed of blood flow in the Internal Carotid Artery relative to the Common Carotid Artery.
A higher ratio suggests that blood is flowing faster through the ICA compared to the CCA.
This increased velocity is often a compensatory mechanism in response to a narrowing or stenosis in the ICA.
The body attempts to maintain adequate blood supply to the brain by accelerating blood flow through the narrowed segment.
Therefore, the ICA/CCA ratio serves as a key indicator of potential carotid artery disease, prompting further investigation and management.
The ICA and CCA: A Basic Anatomy Lesson provided a foundation for understanding how these critical arteries are measured. Now, it's time to translate the numerical results of the ICA/CCA ratio into a clear picture of your vascular health, revealing what these numbers actually signify and, just as importantly, what they don't.
Decoding Your ICA/CCA Results: What Do the Numbers Mean?
The ICA/CCA ratio is not just a random number; it's a key indicator of potential carotid artery disease. Understanding the normal range, how elevated ratios suggest stenosis, and the limitations of this measurement is vital for interpreting your results effectively.
Defining the Normal Range
The normal ICA/CCA ratio is generally considered to be less than 2.0.
This means that the peak systolic velocity (PSV) in the ICA is less than twice the PSV in the CCA.
When the ratio falls within this range, it typically suggests that there is no significant narrowing or blockage in the internal carotid artery. However, it’s crucial to remember that this is just one piece of the puzzle.
Elevated Ratios and Carotid Stenosis
When the ICA/CCA ratio exceeds 2.0, it raises suspicion for carotid stenosis.
An elevated ratio suggests that blood is flowing faster than normal through the ICA, which can happen when the artery is narrowed.
The higher the ratio, the greater the likelihood and severity of the stenosis. Keep in mind that other factors can also impact the ratio.
Correlation Between Ratio Values and Stenosis Severity
The ICA/CCA ratio is often used to estimate the degree of carotid stenosis, categorized as mild, moderate, or severe. While the exact cutoffs may vary slightly between laboratories, here's a general guideline:
- Mild Stenosis: Ratios between 2.0 and 3.0 may indicate mild stenosis (30-49% narrowing).
- Moderate Stenosis: Ratios between 3.0 and 4.0 often suggest moderate stenosis (50-69% narrowing).
- Severe Stenosis: Ratios above 4.0 typically indicate severe stenosis (70-99% narrowing).
It is imperative to recognize that these are general guidelines, and other diagnostic information is necessary for confirmation.
An experienced vascular specialist will correlate these findings with waveform analysis, plaque morphology, and clinical presentation.
Understanding the Ratio’s Limitations
While the ICA/CCA ratio is a valuable tool, it doesn’t provide a complete picture of carotid artery health.
It primarily reflects the peak systolic velocity, which can be influenced by factors other than stenosis.
For example, cardiac output, blood pressure, and the presence of tandem lesions (multiple stenoses in the same artery) can all affect the ratio.
Additionally, the ICA/CCA ratio does not provide information about plaque composition (e.g., whether it is soft or calcified), which can influence the risk of stroke. It also does not visualize the artery directly.
The ICA and CCA: A Basic Anatomy Lesson provided a foundation for understanding how these critical arteries are measured. Now, it's time to translate the numerical results of the ICA/CCA ratio into a clear picture of your vascular health, revealing what these numbers actually signify and, just as importantly, what they don't.
Why Carotid Stenosis Matters: The Stroke Connection
Carotid stenosis isn't just a medical term; it's a critical risk factor for stroke, a life-altering event that can have devastating consequences. Understanding the connection between narrowed carotid arteries and stroke is paramount for proactive health management. Early diagnosis and intervention are key to mitigating this risk.
The Direct Link: Carotid Stenosis and Stroke
When the carotid arteries become significantly narrowed due to plaque buildup (atherosclerosis), the brain's blood supply is compromised. This can lead to stroke in two primary ways:
-
Embolic Stroke: Plaque can rupture or break off from the carotid artery wall, forming an embolus. This embolus travels through the bloodstream and lodges in a smaller artery in the brain, blocking blood flow and causing a stroke.
-
Thrombotic Stroke: Severe stenosis can reduce blood flow to the point where the brain tissue doesn't receive enough oxygen and nutrients, leading to a thrombotic stroke. This is essentially a "traffic jam" within the artery itself.
In either scenario, the result is the same: brain cells deprived of oxygen begin to die, leading to neurological deficits such as weakness, paralysis, speech difficulties, and cognitive impairment. The severity and location of the stroke determine the specific symptoms and long-term impact.
TIAs: Heeding the Warning Signs
Transient Ischemic Attacks (TIAs), often referred to as "mini-strokes," are temporary episodes of neurological dysfunction caused by a brief interruption of blood flow to the brain. TIAs are critical warning signs that a more significant stroke may be imminent.
Symptoms of a TIA are similar to those of a stroke, but they typically resolve within a few minutes to a few hours. These symptoms can include:
- Sudden weakness or numbness in the face, arm, or leg (usually on one side of the body).
- Difficulty speaking or understanding speech.
- Vision loss in one or both eyes.
- Sudden dizziness or loss of balance.
- Severe headache with no known cause.
It's crucial to seek immediate medical attention if you experience any TIA symptoms, even if they resolve quickly. Ignoring these warning signs is like ignoring a fire alarm – it could lead to a catastrophic event. TIAs provide a valuable opportunity for intervention and stroke prevention.
The Urgency of Early Diagnosis and Intervention
The link between carotid stenosis and stroke underscores the importance of early diagnosis and timely intervention. The longer carotid stenosis goes undetected and untreated, the greater the risk of stroke.
Diagnostic tools like duplex ultrasound, CT angiography (CTA), and MR angiography (MRA) can accurately assess the degree of carotid stenosis. Once diagnosed, treatment options range from lifestyle modifications and medication to surgical interventions like carotid endarterectomy (CEA) or carotid artery stenting (CAS).
By proactively addressing carotid stenosis, we can significantly reduce the risk of stroke and protect brain health. This proactive approach requires both awareness of risk factors and a commitment to regular medical check-ups, especially for individuals with a family history of stroke or heart disease.
Why Carotid Stenosis Matters: The Stroke Connection provided a foundation for understanding how these critical arteries are measured. Now, it's time to examine the underlying factors that contribute to the development of carotid stenosis, further illuminating the path toward proactive management and prevention.
Risk Factors: Unveiling the Roots of Carotid Stenosis
Carotid stenosis doesn't arise in a vacuum. It's typically the result of a complex interplay between genetic predispositions and lifestyle choices, gradually accumulating over time. Understanding these contributing factors is crucial for identifying individuals at higher risk and implementing preventive strategies.
The Usual Suspects: Key Modifiable Risk Factors
Several well-established risk factors significantly increase the likelihood of developing carotid stenosis. Fortunately, many of these are modifiable, meaning individuals can actively take steps to mitigate their impact.
-
Hypertension (High Blood Pressure): Chronically elevated blood pressure places undue stress on the arterial walls, accelerating the atherosclerotic process. The constant pressure damages the inner lining of the arteries, making them more susceptible to plaque buildup. Effective management of hypertension through medication and lifestyle changes is paramount.
-
Hyperlipidemia (High Cholesterol): Elevated levels of LDL ("bad") cholesterol contribute directly to the formation of plaque within the arteries. LDL cholesterol accumulates in the arterial walls, triggering inflammation and the development of atherosclerotic lesions. Statins and dietary modifications are key interventions.
-
Smoking: Smoking is a potent vascular toxin, damaging the endothelium (the inner lining of blood vessels) and promoting inflammation. It also increases the risk of blood clot formation and reduces levels of HDL ("good") cholesterol. Smoking cessation is arguably the single most impactful lifestyle change for vascular health.
-
Diabetes: Diabetes is characterized by elevated blood sugar levels, which damage blood vessels throughout the body, including the carotid arteries. This damage accelerates atherosclerosis and increases the risk of carotid stenosis. Careful management of blood sugar levels through diet, exercise, and medication is crucial.
The Cerebrovascular Connection: Beyond the Carotid Arteries
Carotid stenosis is intimately linked to cerebrovascular disease, a broad term encompassing any condition affecting the blood vessels of the brain.
The same risk factors that contribute to carotid stenosis also increase the risk of other cerebrovascular conditions, such as:
-
Cerebral aneurysms
-
Arteriovenous malformations (AVMs)
-
Small vessel disease
This highlights the importance of a holistic approach to vascular health, addressing risk factors that impact the entire cerebrovascular system.
A Wider View: Carotid Stenosis and Overall Cardiovascular Health
Carotid stenosis is often a manifestation of broader cardiovascular disease, indicating underlying problems with the heart and blood vessels throughout the body.
Individuals with carotid stenosis are at increased risk of:
-
Coronary artery disease (CAD): Blockage of the arteries supplying the heart
-
Peripheral artery disease (PAD): Blockage of the arteries supplying the legs and feet
-
Heart attack
-
Stroke
Therefore, managing risk factors for carotid stenosis is not just about preventing stroke, but also about improving overall cardiovascular health and reducing the risk of other serious cardiovascular events. It is a call to action to manage all aspects of your health.
Why Carotid Stenosis Matters: The Stroke Connection provided a foundation for understanding how these critical arteries are measured. Now, it's time to examine the underlying factors that contribute to the development of carotid stenosis, further illuminating the path toward proactive management and prevention.
What's Next? Diagnosis and Treatment Options
An abnormal ICA/CCA ratio from a Duplex Ultrasound is not the end of the road. Instead, it serves as a crucial starting point for further evaluation and, if necessary, treatment. The goal is to accurately determine the degree of stenosis and to implement strategies that minimize the risk of stroke.
The Role of Duplex Ultrasound in Initial Assessment
Duplex Ultrasound is typically the initial non-invasive test used to assess carotid artery stenosis. It utilizes sound waves to visualize the arteries and measure blood flow velocity.
While valuable, it's important to understand that Duplex Ultrasound has limitations. The accuracy can be affected by factors such as the patient's anatomy, the skill of the technician performing the study, and the presence of calcifications in the arteries.
Therefore, depending on the initial findings, further diagnostic testing may be necessary.
When to See a Specialist: Neurologist or Vascular Surgeon
The decision to consult with a specialist depends on several factors, including the severity of the stenosis, the presence of symptoms (such as TIA or stroke), and the individual's overall health status.
Generally, a consultation with a neurologist or vascular surgeon is recommended when the stenosis is moderate (50-69%) or severe (70-99%), especially if the patient is symptomatic. Neurologists specialize in disorders of the nervous system, including stroke prevention. Vascular surgeons specialize in the treatment of blood vessel diseases, including carotid stenosis.
Both specialists can provide expert evaluation and guidance on the most appropriate treatment options. Even in cases of mild stenosis, a specialist referral might be warranted if the patient has multiple risk factors or a strong family history of stroke.
Lifestyle Modifications: The Foundation of Prevention
Regardless of the severity of carotid stenosis, lifestyle modifications play a crucial role in managing the condition and reducing the risk of stroke. These changes focus on addressing modifiable risk factors.
- Diet: A heart-healthy diet low in saturated and trans fats, cholesterol, and sodium is essential. Emphasize fruits, vegetables, whole grains, and lean protein sources.
- Exercise: Regular physical activity helps lower blood pressure, improve cholesterol levels, and maintain a healthy weight. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Smoking Cessation: Quitting smoking is paramount. Smoking damages blood vessels and significantly increases the risk of stroke.
Medical Management: Antiplatelets and Statins
Medications are often prescribed to help manage carotid stenosis and reduce the risk of stroke. The two main categories of drugs used are antiplatelet medications and statins.
- Antiplatelet Medications: These medications, such as aspirin or clopidogrel, help prevent blood clots from forming in the arteries. By reducing the risk of clot formation, they lower the chance of stroke.
- Statins: These medications lower LDL ("bad") cholesterol levels in the blood. Lowering LDL cholesterol helps to slow the progression of atherosclerosis and stabilize existing plaque, reducing the risk of plaque rupture and stroke.
Interventional Procedures: Carotid Endarterectomy (CEA) and Carotid Artery Stenting (CAS)
For individuals with severe carotid stenosis, particularly those who are symptomatic, interventional procedures may be necessary to restore blood flow to the brain. The two main procedures are Carotid Endarterectomy (CEA) and Carotid Artery Stenting (CAS).
Carotid Endarterectomy (CEA)
CEA is a surgical procedure in which the surgeon makes an incision in the neck to directly access the carotid artery. The plaque is then surgically removed from the artery, restoring normal blood flow.
CEA has been the gold standard treatment for severe carotid stenosis for many years, with well-established long-term outcomes.
Carotid Artery Stenting (CAS)
CAS is a minimally invasive procedure in which a catheter is inserted into an artery (usually in the groin) and guided to the carotid artery. A stent, which is a small mesh tube, is then deployed to open up the narrowed artery and improve blood flow.
CAS offers a less invasive alternative to CEA, but it may not be suitable for all patients. The choice between CEA and CAS depends on various factors, including the patient's anatomy, overall health, and the experience of the treating physician.
The decision to pursue treatment isn't always straightforward and should never be undertaken lightly. That's why relying on established treatment guidelines is so essential for informed decision-making and optimal patient outcomes.
The Importance of Treatment Guidelines
In the complex landscape of carotid stenosis management, adhering to established medical guidelines is paramount. These guidelines, developed through rigorous research and expert consensus, provide a framework for diagnosis, treatment, and follow-up care. They are crucial for ensuring that patients receive the most appropriate and effective care based on the best available evidence.
Why Follow Medical Guidelines?
Adhering to medical guidelines ensures consistency and quality in patient care. They minimize variability in treatment approaches and promote the use of evidence-based practices. This leads to better outcomes and reduces the risk of unnecessary or ineffective interventions.
The Role of Expert Organizations
Several professional organizations, such as the Society for Vascular Surgery (SVS), the American Heart Association (AHA), and the American Stroke Association (ASA), develop and publish guidelines for carotid stenosis management.
These guidelines are regularly updated to reflect the latest advances in medical knowledge and technology. They provide healthcare professionals with clear recommendations on:
- When to initiate diagnostic testing.
- Which imaging modalities are most appropriate.
- The optimal treatment strategies for different degrees of stenosis.
- The role of medical management versus interventional procedures.
- Post-treatment surveillance and follow-up.
By consulting these guidelines, physicians can make informed decisions tailored to each patient's unique circumstances.
Specific Examples: SVS Guidelines
The Society for Vascular Surgery (SVS) offers comprehensive guidelines that are frequently referenced in vascular care. These guidelines offer detailed recommendations based on:
- The degree of carotid stenosis.
- The presence or absence of symptoms.
- The patient's overall health status.
For instance, the SVS guidelines provide specific criteria for determining when carotid endarterectomy (CEA) or carotid artery stenting (CAS) is the preferred treatment option. They also outline the recommended medical management strategies, including the use of antiplatelet medications and statins, to reduce the risk of stroke.
Ensuring Optimal Patient Care
Ultimately, the goal of medical guidelines is to optimize patient care and improve outcomes. By providing a standardized approach to diagnosis and treatment, these guidelines help to:
- Reduce the risk of stroke.
- Prevent disease progression.
- Enhance the quality of life for individuals with carotid stenosis.
Healthcare providers who follow these guidelines are better equipped to deliver evidence-based care.
This promotes the best possible outcomes for their patients.
Working with Your Healthcare Team for Optimal Care
Having a clear understanding of your ICA/CCA ratio and potential treatment pathways is essential, but it's only one piece of the puzzle. Navigating the complexities of carotid stenosis management requires a collaborative, multidisciplinary approach.
This means actively engaging with your healthcare team, comprised of your primary care physician, neurologist, and potentially a vascular surgeon, to develop a personalized care plan. This collaborative effort ensures that all aspects of your health are considered, leading to the most effective and appropriate treatment strategy.
The Multidisciplinary Advantage
The management of carotid stenosis is rarely a solitary endeavor. It often requires the combined expertise of multiple specialists. Your primary care physician plays a crucial role in monitoring your overall health, managing risk factors like hypertension and hyperlipidemia, and coordinating your care.
A neurologist specializes in disorders of the nervous system, including the brain and blood vessels. They can assess your neurological symptoms, interpret imaging studies, and determine the impact of carotid stenosis on your brain function.
In cases requiring intervention, a vascular surgeon is essential. These specialists are skilled in performing surgical procedures, such as carotid endarterectomy (CEA), and endovascular procedures, such as carotid artery stenting (CAS), to restore blood flow to the brain.
A multidisciplinary approach ensures comprehensive care by bringing together diverse expertise for optimal patient outcomes.
Fostering Collaboration: The Key to Success
Effective collaboration among your healthcare providers is critical. Your primary care physician should communicate regularly with your neurologist and vascular surgeon to share information about your medical history, medications, and any relevant test results.
Similarly, your neurologist and vascular surgeon should work together to determine the most appropriate treatment strategy based on your individual risk factors, the severity of your stenosis, and your overall health.
Open communication and shared decision-making are essential for successful carotid stenosis management.
This coordinated approach minimizes the risk of conflicting recommendations and ensures that you receive consistent and well-informed care.
Empowering Yourself: Questions to Ask Your Doctor
Taking an active role in your healthcare involves asking informed questions and expressing your concerns. Don't hesitate to seek clarification or additional information from your doctor.
Here are some example questions you might consider asking your healthcare team:
- "What does my ICA/CCA ratio specifically indicate about the severity of my carotid stenosis?"
- "What are the potential risks and benefits of medical management versus interventional procedures (CEA or CAS) in my specific case?"
- "What lifestyle modifications can I make to reduce my risk of stroke and improve my overall vascular health?"
- "What are the specific goals of my treatment plan, and how will we monitor my progress?"
- "What are the potential long-term complications associated with carotid stenosis and its treatment?"
- "Who should I contact if I experience any new or worsening symptoms, such as dizziness, vision changes, or weakness?"
- "How often should I schedule follow-up appointments and imaging studies to monitor my carotid arteries?"
- "Are there any clinical trials or research studies that I might be eligible for?"
Remember, you are a vital member of your healthcare team. Your questions and concerns are important and deserve to be addressed with respect and transparency.
By actively participating in your care and fostering strong communication with your healthcare providers, you can empower yourself to make informed decisions and optimize your vascular health.
Video: ICA/CCA Ratio: What Your Results Really Mean & What's Next
Understanding Your ICA/CCA Ratio: FAQs
Here are some frequently asked questions to help you better understand your ICA/CCA ratio results and what they mean for you.
What does a higher ICA/CCA ratio actually indicate?
A higher ICA/CCA ratio suggests a greater proportion of Intracranial Arteries (ICA) blood flow compared to Common Carotid Arteries (CCA) blood flow. This could indicate increased resistance in the extracranial carotid arteries or increased demand in the intracranial vessels. Further investigation is usually needed to determine the exact cause.
Is there a "normal" ICA/CCA ratio range?
While there isn't a universally accepted "normal" range, typical values are often established by individual labs. Significant deviations from your baseline, or what's considered normal for your age and health profile, are what warrant concern. Consult with your doctor for interpretation.
What factors can influence my ICA/CCA ratio?
Several factors can influence the ica/cca ratio, including age, blood pressure, the presence of carotid artery stenosis (narrowing), and other underlying health conditions. Even body position during the scan can have a minor impact.
What happens after an abnormal ICA/CCA ratio result?
If your ica/cca ratio is outside the expected range, your doctor will likely order additional tests to investigate further. These tests might include carotid ultrasound, CT angiography (CTA), or magnetic resonance angiography (MRA) to visualize the arteries in greater detail and identify any potential problems.