Cephalomedullary Nail: Recovery, Procedure & Risks
A cephalomedullary nail represents a critical orthopedic implant option for addressing complex proximal femur fractures, especially in geriatric patients susceptible to osteoporotic bone. The surgical procedure involving a cephalomedullary nail typically requires specialized training and adherence to strict protocols within a hospital setting to ensure accurate placement and optimal patient outcomes. Rehabilitation protocols following the implantation of a cephalomedullary nail are often guided by physical therapists who help patients regain mobility and strength. Zimmer Biomet is a key manufacturer of these nails, offering various designs to accommodate different fracture patterns and patient anatomies.
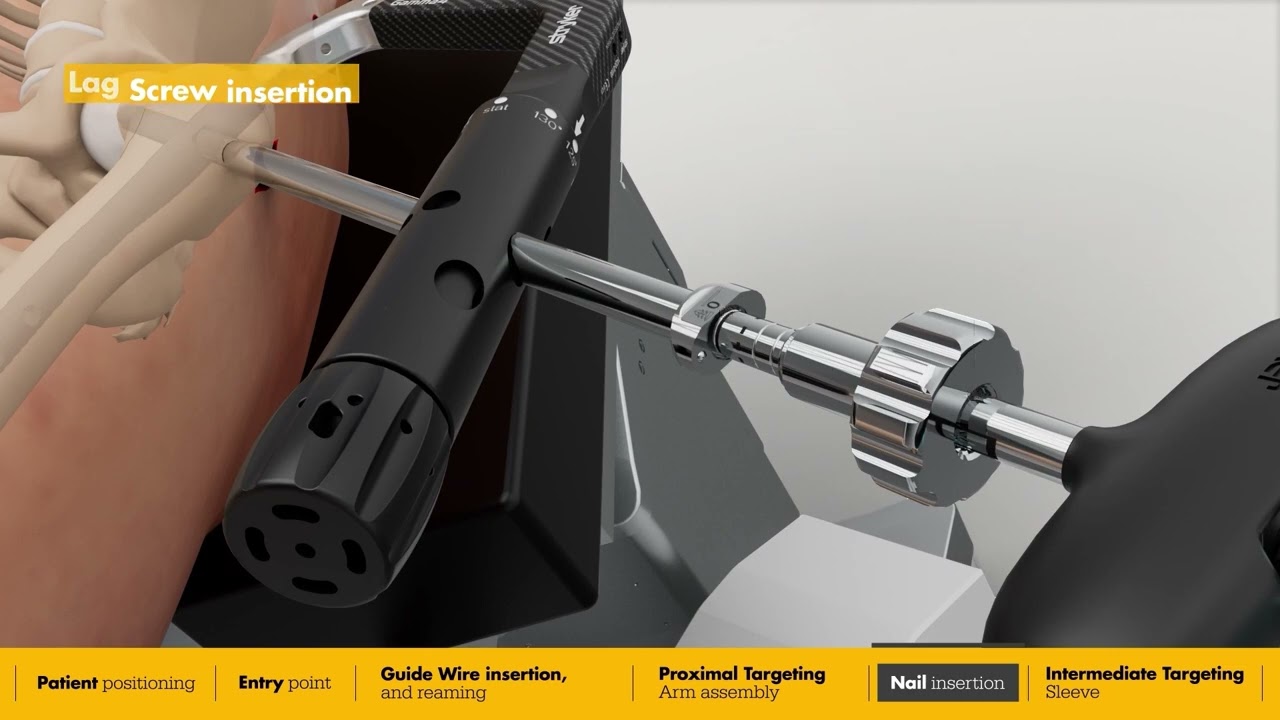
Image taken from the YouTube channel Stryker's clinical solutions , from the video titled Intermediate Nail surgical animation | Gamma4 Hip Fracture Nailing System .
Cephalomedullary nailing stands as a cornerstone in modern orthopedic surgery, offering a robust solution for complex proximal femur fractures. Its significance lies in its ability to provide stable fixation, promoting rapid healing and functional recovery.
What is Cephalomedullary Nailing?
At its core, a cephalomedullary nail is an intramedullary implant designed to stabilize fractures of the proximal femur. The device, typically constructed from titanium or stainless steel, is inserted into the medullary canal of the femur.
Its primary function is to bridge the fracture site, distributing weight-bearing forces along the length of the bone. This reduces stress on the fracture itself. This stabilization is crucial for enabling the body's natural healing processes.
The "cephalo" component refers to the screws or blades that are inserted into the femoral head and neck. This provides additional fixation and prevents rotation or displacement of the fractured segments.
Common Fracture Types Addressed
Cephalomedullary nailing is particularly effective in addressing several common fracture patterns of the proximal femur. These include:
- Femoral Neck Fractures: Fractures occurring in the narrow region connecting the femoral head to the femoral shaft.
- Intertrochanteric Fractures: Fractures located between the greater and lesser trochanters, often characterized by instability.
- Subtrochanteric Fractures: Fractures occurring below the lesser trochanter, extending down the femoral shaft.
The selection of cephalomedullary nailing depends on various factors, including fracture pattern, bone quality, and patient-specific considerations.
Goals of the Procedure
The overarching goals of cephalomedullary nailing extend beyond mere fracture fixation. The ultimate aim is to restore the patient's pre-injury function and quality of life. These goals encompass:
-
Fracture Reduction: Achieving anatomical or near-anatomical alignment of the fractured bone fragments. This is essential for proper healing and biomechanics.
-
Bone Healing: Promoting callus formation and eventual union of the fracture site, leading to a stable and weight-bearing femur.
-
Functional Restoration: Enabling the patient to regain mobility, strength, and range of motion in the affected hip and leg. This involves a comprehensive rehabilitation program.
Anatomy of the Proximal Femur: A Foundation for Understanding
Cephalomedullary nailing's effectiveness hinges on a deep understanding of the proximal femur's intricate anatomy. This region, where the femur connects to the hip, is a complex interplay of bone, muscle attachments, and crucial neurovascular structures.
A surgeon's familiarity with these elements is paramount for successful fracture reduction and stable implant placement. A thorough grasp of proximal femoral anatomy minimizes the risk of complications.
The Femur: Location and Role
The femur, or thigh bone, is the longest and strongest bone in the human body. It extends from the hip to the knee, playing a vital role in weight-bearing, locomotion, and maintaining overall structural integrity.
Its robust architecture is designed to withstand considerable forces, making it essential for everyday activities. Understanding its location and function provides crucial context for appreciating the complexities of proximal femur fractures.
Key Structures of the Proximal Femur
The proximal femur comprises several distinct structures, each with unique anatomical characteristics and biomechanical functions.
The Femoral Head and Acetabulum
The femoral head, a spherical structure at the top of the femur, articulates with the acetabulum.
The acetabulum is a cup-shaped socket in the pelvis.
This ball-and-socket joint allows for a wide range of hip movements, including flexion, extension, abduction, adduction, and rotation. The smooth articulation between these two structures is critical for pain-free hip function.
The Femoral Neck
Connecting the femoral head to the femoral shaft is the femoral neck. This slightly angled segment is a common site for fractures, especially in older adults with osteoporosis.
The femoral neck's angle of inclination is crucial for optimal hip biomechanics.
Fractures in this region can disrupt blood supply to the femoral head. This can lead to avascular necrosis, a severe complication that compromises bone viability.
Greater and Lesser Trochanters
Located at the junction of the femoral neck and shaft are the greater and lesser trochanters.
These are bony prominences that serve as attachment sites for powerful hip muscles.
The greater trochanter, situated laterally, is the insertion point for the gluteus medius and minimus muscles, critical for hip abduction and stability.
The lesser trochanter, located medially, is the attachment site for the iliopsoas muscle, a primary hip flexor. An understanding of these muscle attachments is essential for proper fracture reduction and rehabilitation.
Anatomical Knowledge: The Cornerstone of Surgical Success
A comprehensive understanding of the proximal femur's anatomy is indispensable for surgeons performing cephalomedullary nailing. It is indispensable for accurate fracture reduction. It is indispensable for precise implant placement. And it is indispensable for minimizing complications.
Knowing the spatial relationships between bony structures, muscle attachments, and neurovascular elements allows surgeons to navigate the surgical field with confidence.
Ultimately, a surgeon's expertise in proximal femoral anatomy directly translates to improved patient outcomes. Better patient outcomes mean faster healing, restored function, and a return to an active lifestyle.
Indications and Contraindications: When is Cephalomedullary Nailing Appropriate?
The decision to proceed with cephalomedullary nailing is a critical juncture, demanding a careful weighing of potential benefits against inherent risks. Selecting the right patient for this procedure is as important as the technical execution itself. This section delves into the specific scenarios where cephalomedullary nailing is indicated, while also outlining the conditions that would preclude its use.
Clearly Defined Indications
Cephalomedullary nailing is primarily indicated for the treatment of specific types of proximal femur fractures. Unstable fractures are key candidates for this surgical intervention. The goal is always to restore stability, promote healing, and regain patient mobility.
Primary Indications: Fractures of the Proximal Femur
The most common fractures addressed by cephalomedullary nailing include:
-
Unstable Intertrochanteric Fractures: These fractures occur between the greater and lesser trochanters. Their instability often necessitates surgical intervention.
-
Subtrochanteric Fractures: Located below the lesser trochanter, these fractures present unique challenges due to the high stresses in this region.
-
Certain Femoral Neck Fractures: While hip replacement is often considered for femoral neck fractures, cephalomedullary nailing may be appropriate in specific cases, especially in younger patients or those with certain fracture patterns.
Contraindications: Situations Where the Procedure Is Unsuitable
While cephalomedullary nailing can be a powerful tool, it is not universally applicable. Specific contraindications must be carefully considered to avoid potentially adverse outcomes. Ignoring contraindications can lead to complications and compromise patient safety.
Absolute Contraindications
Certain conditions represent absolute contraindications, meaning the procedure should not be performed under any circumstances:
-
Active Infection at the Surgical Site: The presence of an active infection dramatically increases the risk of postoperative complications, including osteomyelitis. Eradicating the infection is paramount before considering any surgical intervention.
-
Medical Conditions Precluding Safe Surgery: Patients with severe, unmanaged medical conditions may not be able to tolerate the physiological stress of surgery. These conditions must be carefully evaluated and optimized before proceeding.
Relative Contraindications
Relative contraindications require careful consideration and may necessitate modification of the surgical plan or alternative treatment strategies:
-
Severe Osteoporosis: Severely osteoporotic bone may not provide adequate fixation for the cephalomedullary nail, increasing the risk of implant failure.
-
Significant Comorbidities: The presence of multiple or severe comorbidities increases the risk of complications and may impact the patient's ability to recover fully. A comprehensive risk-benefit analysis is essential.
The Importance of Patient Selection
The meticulous assessment of indications and contraindications is paramount for achieving optimal patient outcomes. Failing to carefully consider these factors can lead to complications, delayed healing, and suboptimal functional results. The decision to proceed with cephalomedullary nailing should be made collaboratively by the surgeon, the patient, and other members of the healthcare team, ensuring a patient-centered approach.
Pre-operative Planning: The Cornerstone of Successful Cephalomedullary Nailing
The decision to proceed with cephalomedullary nailing is a critical juncture, demanding a careful weighing of potential benefits against inherent risks. Selecting the right patient for this procedure is as important as the technical execution itself. This section delves into the crucial steps of pre-operative planning, highlighting how meticulous preparation significantly contributes to a successful surgical outcome.
Comprehensive Patient Evaluation: Assessing Suitability
Before any incision is made, a thorough patient evaluation is paramount. This goes beyond simply identifying the fracture; it involves a holistic assessment of the patient's overall health and their ability to withstand the rigors of surgery and subsequent rehabilitation.
-
Medical History: A detailed review of the patient's medical history is crucial. Pre-existing conditions, such as cardiovascular disease, diabetes, or respiratory issues, can significantly impact surgical risk and recovery.
These conditions must be carefully managed and optimized before proceeding.
-
Medication Review: A comprehensive medication review is essential. Certain medications, such as anticoagulants or antiplatelet agents, can increase the risk of bleeding during and after surgery.
These medications may need to be adjusted or discontinued prior to the procedure, under the guidance of the patient's primary care physician.
-
Physical Examination: A thorough physical examination helps assess the patient's overall physical condition and identify any potential contraindications to surgery. This includes evaluating skin integrity at the proposed surgical site, assessing peripheral circulation, and documenting any neurological deficits.
Careful attention to detail during the physical exam can help anticipate and mitigate potential complications.
The Indispensable Role of Imaging: X-rays and Radiographic Interpretation
Imaging studies, particularly X-rays, are the cornerstone of pre-operative planning for cephalomedullary nailing. These images provide crucial information about the fracture pattern, the degree of displacement, and the overall bone quality.
-
Fracture Pattern Assessment: X-rays allow the surgeon to meticulously analyze the fracture pattern. This includes identifying the type of fracture (e.g., intertrochanteric, subtrochanteric, femoral neck), the number of fracture fragments, and the presence of any comminution (multiple fracture lines).
Understanding the fracture pattern is essential for selecting the appropriate implant and planning the surgical approach.
-
Angulation and Displacement: Radiographs accurately quantify the degree of angulation and displacement of the fracture fragments. This information guides the surgeon in determining the optimal reduction technique and ensuring proper alignment of the bone.
Precise measurement and appreciation of angulation and displacement reduces the risks of malunion and non-union.
-
Radiologist Expertise: The radiologist plays a pivotal role in interpreting the imaging studies. Their expertise in identifying subtle fracture lines, assessing bone density, and detecting any pre-existing abnormalities is invaluable. The radiologist's report provides the surgeon with a comprehensive overview of the fracture characteristics, enabling informed decision-making.
-
Advanced Imaging: In certain complex cases, advanced imaging modalities such as CT scans or MRI may be necessary. These studies provide more detailed information about the fracture anatomy, the presence of soft tissue injuries, and the overall bone quality.
The responsible use of advanced imaging improves patient outcomes.
The Direct Correlation Between Planning and Surgical Success
Meticulous pre-operative planning is not merely a formality; it is a fundamental determinant of surgical success. By thoroughly evaluating the patient, carefully analyzing the imaging studies, and anticipating potential challenges, the surgeon can optimize the surgical approach, minimize complications, and enhance the likelihood of a successful outcome.
A well-executed pre-operative plan translates to:
- Reduced Surgical Time: A clear understanding of the fracture pattern and the surgical approach allows for a more efficient and streamlined surgical procedure, minimizing operative time.
- Improved Fracture Reduction: Precise pre-operative planning facilitates accurate fracture reduction, ensuring proper alignment of the bone and promoting optimal healing.
- Minimized Complications: By identifying potential risk factors and anticipating challenges, pre-operative planning helps minimize the risk of complications such as malunion, nonunion, and infection.
- Enhanced Patient Outcomes: Ultimately, meticulous pre-operative planning leads to improved patient outcomes, with faster recovery, reduced pain, and a return to functional activity.
Surgical Technique: A Step-by-Step Guide
Pre-operative planning and the meticulous assessment of patient-specific factors lay the groundwork for a successful cephalomedullary nailing procedure. The true test, however, lies in the precise execution of the surgical technique itself. This section provides a detailed overview of the cephalomedullary nailing procedure.
Assembling the Surgical Team
The success of any surgical endeavor hinges on the synergy of a skilled and coordinated team. In cephalomedullary nailing, the core team comprises:
-
The Orthopedic Surgeon: The linchpin of the operation, the orthopedic surgeon bears ultimate responsibility for surgical planning, fracture reduction, nail implantation, and post-operative management. Their expertise dictates the overall trajectory of the procedure.
-
The Anesthesiologist: Beyond managing anesthesia, the anesthesiologist plays a crucial role in monitoring the patient's physiological status throughout the surgery. They are responsible for administering medications and managing pain levels.
-
Operating Room Nurses: Highly skilled and versatile, nurses are the backbone of the operating room. They provide essential support to the surgeon, prepare instruments, monitor the patient's condition, and ensure a sterile surgical environment.
Patient Positioning: Setting the Stage
Precise patient positioning is paramount to achieving optimal surgical access and visualization. Typically, the patient is placed in the supine position on a fracture table. This specialized table allows for traction and rotation, facilitating fracture reduction. The affected limb is carefully positioned to allow for unobstructed fluoroscopic imaging.
Fracture Reduction: Restoring Anatomical Alignment
The primary objective of fracture reduction is to restore the fractured bone fragments to their pre-injury anatomical alignment. Achieving adequate reduction is vital for ensuring optimal bone healing and functional outcomes. Two primary techniques are employed:
Closed Reduction Internal Fixation (CRIF)
This minimally invasive technique aims to reduce the fracture without making a large incision.
Using external manipulation and traction, the surgeon attempts to realign the bone fragments. Fluoroscopy plays a crucial role in visualizing the fracture and guiding the reduction maneuver.
Once an acceptable reduction is achieved, it is maintained using temporary fixation, such as guide wires or pins, before proceeding with nail insertion.
Open Reduction Internal Fixation (ORIF)
In cases where closed reduction proves inadequate, open reduction becomes necessary. This involves making an incision to directly visualize the fracture site.
The surgeon then manually manipulates the bone fragments into their correct anatomical position.
Once reduced, the fragments are temporarily held in place with clamps or sutures. This allows for the subsequent insertion of the cephalomedullary nail and associated screws.
Implantation Process: Securing the Fracture
The cornerstone of cephalomedullary nailing lies in the precise implantation of the nail. This intricate process involves several key steps:
Insertion of Guide Wires
Guide wires serve as the roadmap for nail insertion. These thin, flexible wires are carefully advanced through the entry point in the greater trochanter. This is done under fluoroscopic guidance, down the intramedullary canal of the femur, across the fracture site, and into the femoral head. Precise placement of the guide wires is essential for ensuring accurate nail positioning.
Placement of the Cephalomedullary Nail
The cephalomedullary nail is a specially designed implant. It is engineered to fit within the intramedullary canal of the femur.
It is advanced over the guide wire and carefully impacted into place. The nail spans the fracture site, providing stability and promoting healing.
Nail selection is based on pre-operative planning. It accounts for the patient's anatomy and the specific fracture pattern.
Drilling for Screw Insertion
Once the nail is properly positioned, precise screw placement becomes crucial. Specialized drill guides are used to create channels through the nail and into the bone. The drill guides ensure that the screws are inserted at the correct angle and depth to achieve optimal fixation.
Insertion of Lag Screws and Locking Screws
Lag screws are inserted through the nail and into the femoral head, compressing the fracture fragments together. This compression enhances stability and promotes bone healing. Locking screws are then placed through the nail.
This locks it to the femoral shaft, providing additional stability and preventing rotation or migration of the implant. The number and placement of screws are determined by the fracture pattern and surgeon preference.
Intraoperative Imaging (Fluoroscopy): Real-Time Guidance
Fluoroscopy, a form of real-time X-ray, is indispensable throughout the cephalomedullary nailing procedure. It provides the surgeon with continuous visual feedback. This ensures accurate fracture reduction, guide wire placement, nail positioning, and screw insertion.
Fluoroscopy minimizes the need for extensive surgical exposure. It enhances precision and reduces the risk of complications.
The surgical technique involved in cephalomedullary nailing is a complex interplay of anatomical knowledge, surgical skill, and technological precision. A thorough understanding of each step is critical for achieving optimal patient outcomes.
Post-operative Management: Ensuring a Smooth Recovery
Pre-operative planning and the meticulous assessment of patient-specific factors lay the groundwork for a successful cephalomedullary nailing procedure. The true test, however, lies in the precise execution of the surgical technique itself. From there, attention shifts to the crucial post-operative period. This section provides a detailed overview of the cephalomedullary nailing procedure and the multifaceted approach required to ensure optimal healing and functional recovery.
Immediate Post-operative Care and Monitoring
The initial hours and days following cephalomedullary nailing are critical for establishing a foundation for successful recovery. Vigilant monitoring of vital signs is paramount to detect any immediate post-operative complications. Attention is given to the patient's respiratory and cardiovascular status, as well as neurological function.
Pain management is a key priority, employing a multimodal approach to minimize discomfort and facilitate early mobilization. Wound care is essential to prevent infection. The surgical site is carefully inspected for signs of redness, swelling, or drainage.
Pain Management Protocols
Effective pain management is not merely about patient comfort; it plays a vital role in facilitating early mobilization and preventing complications. Typically managed by nurses under the anesthesiologist's guidance, pain management strategies often involve a combination of:
- Opioid analgesics
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Local anesthetics
The goal is to achieve adequate pain relief while minimizing the risk of side effects. The rise in opioid addiction also forces the medical team to exercise care and caution. Patient-controlled analgesia (PCA) may be used to empower patients to manage their pain effectively.
Wound Care and Infection Prevention
Meticulous wound care is essential to minimize the risk of surgical site infection (SSI). Strict adherence to sterile technique during dressing changes is paramount. Healthcare providers must educate patients on proper wound care procedures to follow at home.
Patients must be instructed to monitor for any signs of infection, such as:
- Increased pain
- Redness
- Swelling
- Drainage
- Fever
Prompt reporting of these symptoms to the surgical team is essential for early intervention and treatment.
The Cornerstone of Recovery: Rehabilitation
Rehabilitation forms the cornerstone of recovery following cephalomedullary nailing. A structured physical therapy program is essential to regain strength, mobility, and function. The physical therapist (PT) plays a crucial role in designing and implementing individualized exercise programs tailored to each patient's specific needs and goals.
The Role of the Physical Therapist (PT)
The PT conducts a thorough assessment to evaluate range of motion, strength, balance, and gait. Based on this assessment, the PT develops a progressive exercise program that gradually increases in intensity and complexity. Exercises may include:
- Range-of-motion exercises
- Strengthening exercises
- Balance training
- Gait training
The PT provides guidance and support throughout the rehabilitation process, helping patients to achieve their functional goals.
Weight-Bearing Restrictions
Weight-bearing restrictions are an integral part of the rehabilitation process, dictated by the orthopedic surgeon based on fracture stability and bone healing. Adherence to these restrictions is crucial to prevent complications such as implant failure or delayed union. Patients must be educated on the appropriate use of assistive devices, such as crutches or walkers, to maintain the prescribed weight-bearing status.
Weight-bearing restrictions are categorized as:
- Non-weight-bearing (NWB)
- Touch-down weight-bearing (TDWB)
- Partial weight-bearing (PWB)
- Weight-bearing as tolerated (WBAT)
- Full weight-bearing (FWB)
Patient Adherence: The Key to Optimal Healing
Ultimately, the success of post-operative management hinges on patient adherence to instructions. Patients must be educated on the importance of:
- Following medication regimens
- Attending physical therapy appointments
- Adhering to weight-bearing restrictions
- Maintaining proper wound care
Open communication between the patient, surgical team, and physical therapist is essential to address any concerns and optimize the recovery process. A proactive and engaged patient is far more likely to achieve a successful outcome.
Potential Complications: Recognizing and Addressing Risks
Post-operative Management: Ensuring a Smooth Recovery Pre-operative planning and the meticulous assessment of patient-specific factors lay the groundwork for a successful cephalomedullary nailing procedure. The true test, however, lies in the precise execution of the surgical technique itself. From there, attention shifts to the crucial post-operative phase and, critically, to the potential complications that, despite the best efforts, can arise. Recognizing these risks and having a plan to address them is paramount to ensuring the best possible patient outcome.
Cephalomedullary nailing, while a highly effective treatment for proximal femur fractures, is not without potential complications. These can be broadly categorized as early or late, depending on when they manifest following the procedure. A proactive approach to identifying and managing these complications is vital.
Early Complications: Immediate Post-operative Concerns
Early complications typically occur within the first few weeks following surgery. Prompt recognition and intervention are essential to prevent long-term sequelae.
Surgical Site Infection (SSI)
Surgical site infections represent a significant risk in any surgical procedure. SSIs can range from superficial wound infections to deep infections involving the bone and hardware.
Signs of SSI include:
- Increased pain
- Redness
- Swelling
- Drainage from the incision site
- Fever
Treatment typically involves antibiotics and, in severe cases, surgical debridement to remove infected tissue. Adherence to strict sterile techniques during surgery and meticulous wound care post-operatively are crucial preventative measures.
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
Deep vein thrombosis, the formation of blood clots in the deep veins, typically of the legs, is a significant risk following orthopedic surgery. These clots can dislodge and travel to the lungs, causing a pulmonary embolism, a potentially life-threatening condition.
Symptoms of DVT include:
- Swelling
- Pain
- Warmth in the affected leg
Symptoms of PE include:
- Sudden shortness of breath
- Chest pain
- Coughing up blood
Prevention strategies include:
- Anticoagulation medication (blood thinners)
- Mechanical prophylaxis (compression stockings)
- Early mobilization. Early ambulation is key!
Prompt diagnosis and treatment with anticoagulants are critical in managing DVT and PE.
Late Complications: Long-Term Challenges
Late complications manifest months or even years after the initial surgery. These can have a significant impact on long-term function and quality of life.
Malunion
Malunion refers to the fracture healing in a non-anatomical position. This can lead to:
- Pain
- Deformity
- Limited range of motion
The risk of malunion can be minimized through:
- Accurate fracture reduction during the initial surgery
- Appropriate fixation techniques.
Corrective osteotomy, a surgical procedure to re-break and realign the bone, may be necessary in severe cases.
Nonunion
Nonunion occurs when the fracture fails to heal. This can result in persistent pain, instability, and the inability to bear weight.
Factors contributing to nonunion include:
- Inadequate blood supply
- Infection
- Instability at the fracture site
- Patient-related factors (e.g., smoking, diabetes)
Treatment options include:
- Bone grafting to stimulate healing
- Revision surgery to improve stability
- Addressing underlying factors that may be impeding healing
Avascular Necrosis (AVN)
Avascular necrosis, also known as osteonecrosis, occurs when the blood supply to the femoral head is disrupted, leading to bone death. This can result in:
- Pain
- Collapse of the hip joint
- Progressive arthritis
AVN is more common following femoral neck fractures, particularly those that are displaced.
Treatment options range from:
- Pain management to total hip arthroplasty (hip replacement), depending on the severity of the condition.
The Importance of Vigilance and Prompt Intervention
While cephalomedullary nailing is a powerful tool in fracture management, a thorough understanding of potential complications is crucial. Vigilant monitoring, early recognition of warning signs, and prompt intervention are essential for optimizing patient outcomes and minimizing the long-term impact of these complications. A collaborative approach between the surgical team, the patient, and rehabilitation specialists is key to ensuring the best possible recovery.
The Multidisciplinary Team: Orchestrating a Successful Outcome in Cephalomedullary Nailing
Pre-operative planning and the meticulous assessment of patient-specific factors lay the groundwork for a successful cephalomedullary nailing procedure. The true test, however, lies in the precise execution of the surgical technique itself, and the comprehensive care that follows. This entire process is not the work of a single individual, but rather the carefully coordinated effort of a diverse and highly skilled multidisciplinary team.
The success of cephalomedullary nailing hinges on the seamless integration of expertise from various medical disciplines. Each professional brings a unique skillset and perspective to the table, working in concert to optimize patient outcomes.
This collaborative approach ensures that all aspects of patient care, from initial diagnosis to long-term rehabilitation, are addressed with the utmost precision and attention to detail. Let's examine the crucial roles of these key players:
The Orthopedic Surgeon: The Architect of Surgical Intervention
The orthopedic surgeon stands as the central figure in the cephalomedullary nailing process. They are responsible for:
- The initial assessment of the patient.
- Determining the suitability of cephalomedullary nailing.
- Developing the surgical plan.
Most importantly, they are the ones responsible for executing the surgical procedure itself.
The surgeon's expertise in fracture reduction, implant placement, and intraoperative decision-making is paramount to achieving optimal fracture fixation and minimizing the risk of complications. Beyond the operating room, the orthopedic surgeon continues to oversee the patient's post-operative care.
This includes:
- Monitoring the healing process.
- Adjusting the rehabilitation plan as needed.
- Addressing any complications that may arise.
The Radiologist: Illuminating the Path to Diagnosis and Treatment
The radiologist plays a critical, though often unseen, role in cephalomedullary nailing. Their expertise in interpreting radiographic images is essential for accurate diagnosis and surgical planning.
Specifically, the radiologist helps in:
- Identifying the fracture pattern.
- Assessing bone quality.
- Ruling out other potential sources of pain or injury.
During the surgical procedure, the radiologist (or a trained technician under their supervision) operates fluoroscopic imaging equipment. This provides real-time visualization of the fracture site and guides the surgeon in implant placement.
Post-operatively, radiographs are used to assess fracture healing and monitor for any signs of implant failure or other complications. The radiologist's ability to accurately interpret these images is crucial for guiding subsequent treatment decisions.
The Physical Therapist: Guiding the Journey to Recovery
The physical therapist (PT) is instrumental in restoring function and mobility following cephalomedullary nailing. They develop and implement individualized rehabilitation programs designed to:
- Strengthen weakened muscles.
- Improve range of motion.
- Restore weight-bearing capacity.
The PT works closely with the patient to set realistic goals and track progress. They also provide education on proper body mechanics, pain management techniques, and strategies for preventing future injuries.
The rehabilitation process typically involves a gradual progression of exercises, starting with gentle range-of-motion exercises and progressing to more challenging strengthening and balance activities. The PT carefully monitors the patient's response to treatment and adjusts the program accordingly.
Nursing Staff: The Bedrock of Patient Care
Nurses are the backbone of patient care throughout the cephalomedullary nailing process. They provide:
- Essential support.
- Monitoring.
- Education to patients and their families.
Pre-operatively, nurses prepare the patient for surgery, ensuring that they understand the procedure and what to expect during the recovery period. Post-operatively, nurses closely monitor the patient's vital signs, manage pain, and provide wound care.
They also play a crucial role in preventing complications, such as infection and deep vein thrombosis. Nurses are often the first point of contact for patients with questions or concerns. Their compassionate care and attention to detail are essential for ensuring a smooth and comfortable recovery.
In conclusion, cephalomedullary nailing is a complex procedure that requires the coordinated efforts of a multidisciplinary team. The expertise of the orthopedic surgeon, radiologist, physical therapist, and nursing staff is essential for achieving optimal patient outcomes. By working together seamlessly, these professionals can help patients regain function, mobility, and a return to a fulfilling life.
Rehabilitation and Recovery: Regaining Function and Mobility
The success of cephalomedullary nailing hinges not only on the precision of the surgical procedure itself, but also, and perhaps even more significantly, on the patient's commitment to a structured and diligent rehabilitation program. This phase is paramount in restoring function, rebuilding strength, and ensuring a return to a fulfilling and active lifestyle.
The Critical Role of Rehabilitation
Rehabilitation after cephalomedullary nailing is not merely a supplementary component; it is an integral part of the overall treatment strategy. The goals are multifaceted, including:
- Minimizing pain and swelling.
- Restoring range of motion in the hip and knee.
- Strengthening the muscles surrounding the hip and thigh.
- Improving balance and coordination.
- Facilitating a safe return to functional activities.
Neglecting rehabilitation can significantly compromise the outcome of the surgery, leading to persistent pain, limited mobility, and a reduced quality of life.
Adherence to Weight-Bearing Restrictions: A Foundation for Healing
One of the most crucial aspects of the initial recovery period is strict adherence to weight-bearing restrictions. The orthopedic surgeon will determine the appropriate weight-bearing protocol based on the fracture pattern, bone quality, and stability of the fixation.
Common weight-bearing classifications include:
- Non-weight-bearing (NWB): No weight is allowed on the operated leg.
- Touch-down weight-bearing (TDWB): The foot can touch the ground for balance, but no weight is applied.
- Partial weight-bearing (PWB): A limited amount of weight is allowed on the operated leg, typically 20-50% of body weight.
- Weight-bearing as tolerated (WBAT): The patient can gradually increase weight-bearing as comfort allows.
- Full weight-bearing (FWB): Full weight can be placed on the operated leg.
Prematurely increasing weight-bearing can jeopardize the healing process, potentially leading to implant failure, fracture displacement, or delayed union. Patience and diligence are key during this phase.
The Importance of Physical Therapy
Regular physical therapy visits are essential for a successful recovery. A qualified physical therapist will develop a personalized rehabilitation program tailored to the individual patient's needs and goals.
Components of a Physical Therapy Program
A comprehensive physical therapy program typically includes:
- Range-of-motion exercises: To restore flexibility and mobility in the hip and knee.
- Strengthening exercises: To rebuild muscle strength in the hip, thigh, and core.
- Gait training: To improve walking pattern and balance.
- Balance and coordination exercises: To enhance stability and prevent falls.
- Pain management techniques: To alleviate pain and discomfort.
- Functional training: To practice activities of daily living, such as walking, climbing stairs, and getting in and out of a chair.
The physical therapist will also provide education on proper body mechanics, joint protection strategies, and home exercise programs.
Tips for Optimizing Your Recovery
While professional guidance is crucial, patients can also play an active role in optimizing their recovery:
- Follow your surgeon's and physical therapist's instructions meticulously.
- Maintain a healthy diet rich in protein and calcium to promote bone healing.
- Stay hydrated by drinking plenty of water.
- Manage pain effectively with prescribed medications or other pain relief techniques.
- Get adequate rest to allow your body to heal.
- Avoid smoking, as it can impair bone healing.
- Attend all scheduled follow-up appointments.
- Be patient and persistent – recovery takes time and effort.
- Communicate openly with your healthcare team about any concerns or challenges you may be experiencing.
By actively participating in your rehabilitation and adhering to the recommendations of your healthcare team, you can significantly enhance your chances of a successful recovery and a return to a fulfilling and active life.
Video: Cephalomedullary Nail: Recovery, Procedure & Risks
Frequently Asked Questions: Cephalomedullary Nail
What is the main purpose of a cephalomedullary nail?
A cephalomedullary nail is primarily used to stabilize and heal fractures of the femur (thigh bone) that occur near the hip or upper thigh. It provides internal support while the bone mends.
How is a cephalomedullary nail inserted during surgery?
The procedure involves making a small incision near the hip or upper thigh. A guide wire is inserted into the femur, and the cephalomedullary nail is then carefully placed over the wire and advanced into the bone. Screws are inserted through the nail to lock it in place and secure the fracture.
What can I expect during the recovery period after cephalomedullary nail surgery?
Recovery varies, but generally involves pain management, physical therapy to regain strength and mobility, and weight-bearing restrictions initially. Full recovery and return to normal activities can take several months. Following post-operative instructions diligently is key for optimal healing with a cephalomedullary nail.
What are some potential risks associated with a cephalomedullary nail?
Potential risks include infection, non-union (failure of the fracture to heal), malunion (improper healing), implant failure (breakage or loosening of the nail or screws), and irritation around the incision site. Nerve or blood vessel damage is also possible, but less common, after a cephalomedullary nail procedure.
So, there you have it – a rundown on the cephalomedullary nail procedure. Recovery can be a bit of a journey, but with proper care and a good dose of patience, most people are back on their feet before you know it. Don't hesitate to chat with your doctor about any concerns; they're the best resource to guide you through the process and help you understand if a cephalomedullary nail is the right choice for your specific situation.
