Rosuvastatin vs Atorvastatin: Which Is Best For You?
Understanding cardiovascular health involves navigating treatment options like statins. Rosuvastatin, a potent statin, exhibits effectiveness in lowering LDL cholesterol. Atorvastatin, another widely prescribed statin, offers a similar benefit profile. The crucial decision between rosuvastatin vs atorvastatin requires careful consideration, factoring in individual patient profiles and guidelines from organizations like the American Heart Association.

Image taken from the YouTube channel Radcliffe Cardiology , from the video titled ESC 23: LODESTAR: Rosuvastatin Vs Atorvastatin Treatment For CAD Patients .
In the landscape of cardiovascular health, statins stand as cornerstones in the prevention and management of heart disease. Among the various statins available, rosuvastatin (Crestor) and atorvastatin (Lipitor) are two of the most frequently prescribed medications.
Understanding the Role of Statins
Rosuvastatin, known by its brand name Crestor, and atorvastatin, commonly known as Lipitor, belong to a class of drugs called HMG-CoA reductase inhibitors—more simply known as statins. These medications work primarily by inhibiting the production of cholesterol in the liver.
By reducing cholesterol production, statins effectively lower the levels of low-density lipoprotein (LDL) cholesterol, often referred to as "bad" cholesterol, in the bloodstream. Elevated LDL cholesterol is a significant risk factor for the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
Managing Cholesterol and Reducing CVD Risk
The primary function of both rosuvastatin and atorvastatin is to manage cholesterol levels and, consequently, reduce the risk of cardiovascular disease (CVD). High cholesterol, particularly elevated LDL cholesterol, contributes to the formation of arterial plaques, leading to conditions such as heart attack and stroke.
Statins help to stabilize these plaques, reducing the likelihood of rupture and subsequent cardiovascular events.
Navigating Your Statin Choice: An Objective Comparison
Choosing between rosuvastatin and atorvastatin can be a complex decision, as both medications have distinct characteristics and potential benefits. This article aims to provide an objective comparison of these two statins, examining their mechanisms of action, efficacy, side effects, and other relevant factors.
The goal is to empower readers with the information necessary to understand which medication may be more suitable for their individual needs.
It is crucial to emphasize that this information is not a substitute for professional medical advice. The decision to start or change statin therapy should always be made in consultation with a qualified healthcare professional who can assess your specific health status and risk factors.
Navigating Your Statin Choice: An Objective Comparison
Choosing between rosuvastatin and atorvastatin can be a complex decision, as both medications have distinct characteristics and potential benefits. This article aims to provide an objective comparison of these two statins, examining their mechanisms of action, efficacy, side effects, and other relevant factors.
The goal is to empower readers with the knowledge needed to engage in informed discussions with their healthcare providers, ultimately contributing to personalized treatment plans tailored to their unique needs. Before diving into the specifics of each medication, it's essential to establish a solid understanding of statins and their role in managing cholesterol.
Understanding Statins and Cholesterol: A Foundation for Informed Decisions
Statins are a class of drugs that play a pivotal role in managing cholesterol levels and reducing the risk of cardiovascular disease. To truly grasp their significance, it's important to understand how they work and their impact on various types of cholesterol.
The Role of Statins in Lowering LDL Cholesterol
Statins primarily function by inhibiting an enzyme called HMG-CoA reductase, which is crucial in the liver's production of cholesterol.
By blocking this enzyme, statins effectively reduce the amount of cholesterol the liver produces. This, in turn, leads to a decrease in low-density lipoprotein (LDL) cholesterol, often referred to as "bad" cholesterol, in the bloodstream.
Lowering LDL cholesterol is a cornerstone of cardiovascular disease prevention, as elevated levels contribute to the formation of plaque in arteries.
The Significance of LDL, HDL, and Triglycerides
When assessing cardiovascular health, healthcare providers often look at a panel of blood lipids, including LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides.
LDL Cholesterol: As mentioned earlier, LDL cholesterol is a primary culprit in the development of atherosclerosis. High levels promote the buildup of plaque, narrowing arteries and increasing the risk of heart attack and stroke.
HDL Cholesterol: HDL cholesterol, often called "good" cholesterol, helps remove LDL cholesterol from the arteries, transporting it back to the liver for processing. Higher levels of HDL cholesterol are generally associated with a lower risk of heart disease.
Triglycerides: Triglycerides are another type of fat in the blood. While not directly targeted by statins, elevated triglyceride levels can also contribute to cardiovascular risk, especially when combined with high LDL cholesterol and low HDL cholesterol.
How Statins Stabilize Plaque
Beyond lowering LDL cholesterol, statins also possess properties that help stabilize existing plaque in arteries.
These medications can reduce inflammation within the plaque, making it less likely to rupture and cause a sudden cardiovascular event such as a heart attack or stroke.
By stabilizing plaque, statins provide an additional layer of protection against the dangers of atherosclerosis. While lifestyle modifications are key for cardiovascular health, statins offer crucial intervention for individuals at elevated risk.
Understanding the crucial role statins play in managing cholesterol sets the stage for a closer examination of specific medications within this class. We now turn our attention to rosuvastatin, sold under the brand name Crestor, to understand its unique characteristics and how it contributes to cardiovascular health.
Rosuvastatin (Crestor) - A Deep Dive into its Mechanism and Efficacy
Rosuvastatin (Crestor) stands as a potent statin widely prescribed to manage cholesterol levels and mitigate the risk of cardiovascular events. Understanding its mechanism, dosage, and proven efficacy is crucial for both healthcare professionals and patients.
Mechanism of Action: Selectively Targeting Cholesterol Production
Rosuvastatin, like other statins, functions by inhibiting the HMG-CoA reductase enzyme. This enzyme is essential for cholesterol synthesis in the liver.
However, rosuvastatin exhibits a higher affinity for this enzyme compared to some other statins. This enhanced affinity contributes to its potent LDL-C lowering effect.
By blocking HMG-CoA reductase, rosuvastatin reduces the production of cholesterol in the liver. This, in turn, prompts the liver to draw more LDL cholesterol from the bloodstream, effectively lowering LDL-C levels.
Dosage Strengths and Administration: Tailoring Treatment to Individual Needs
Rosuvastatin is available in various dosage strengths, typically ranging from 5 mg to 40 mg.
The starting dose is usually determined by individual cholesterol levels, cardiovascular risk factors, and overall health status.
Higher doses are generally reserved for patients requiring more aggressive LDL-C lowering.
Rosuvastatin is administered orally, usually once daily, and can be taken with or without food. Consistent timing is recommended to maintain stable drug levels in the body.
Efficacy: Robust Clinical Trial Data Supporting LDL-C Reduction
Clinical trials have consistently demonstrated rosuvastatin's efficacy in reducing LDL cholesterol.
Studies have shown that rosuvastatin can achieve significant LDL-C reductions compared to other statins at comparable doses.
Furthermore, rosuvastatin has been shown to increase HDL cholesterol ("good" cholesterol) and lower triglycerides, contributing to a more favorable lipid profile.
Landmark Studies and Key Findings
The JUPITER trial (Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin) stands out as a landmark study.
It demonstrated that rosuvastatin significantly reduced the risk of major cardiovascular events, including heart attack and stroke, in individuals with elevated C-reactive protein (CRP) and normal LDL-C levels.
This finding expanded the understanding of statin benefits beyond traditional cholesterol management.
The ASTEROID trial (A Study To Evaluate the Effect of Rosuvastatin On Intravascular Ultrasound-Derived Coronary Atheroma Burden) further revealed that rosuvastatin could halt or even reverse the progression of atherosclerosis (plaque buildup) in coronary arteries.
This regression was observed through intravascular ultrasound imaging, providing direct evidence of rosuvastatin's impact on plaque burden.
Considerations Regarding High-Intensity Statin Therapy
Rosuvastatin, particularly at higher doses (20-40mg), is often considered a high-intensity statin.
High-intensity statin therapy is typically recommended for patients at very high risk of cardiovascular events.
While highly effective, higher doses may also increase the risk of side effects.
Therefore, careful monitoring and individualized risk-benefit assessments are crucial when prescribing rosuvastatin, especially at higher dosages.
Understanding the effects and function of rosuvastatin provides a basis for comparison. Next, we turn our attention to another widely used statin, atorvastatin, exploring its distinct characteristics and clinical profile.
Atorvastatin (Lipitor) - Unveiling its Mechanism and Efficacy
Atorvastatin, commonly known by its brand name Lipitor, is a cornerstone medication in the management of high cholesterol and the prevention of cardiovascular diseases. Like rosuvastatin, it belongs to the statin class, but understanding its specific properties is key to appreciating its role in patient care.
Mechanism of Action: Targeting Cholesterol Synthesis
Atorvastatin functions by inhibiting HMG-CoA reductase, a crucial enzyme in the cholesterol synthesis pathway within the liver.
By blocking this enzyme, atorvastatin reduces the liver's cholesterol production.
This reduction prompts the liver to uptake more LDL cholesterol from the bloodstream, leading to a decrease in circulating LDL-C levels.
While sharing the same mechanism as other statins, atorvastatin's efficacy and specific interactions can differ, influencing its suitability for certain patients.
Dosage Strengths and Administration
Atorvastatin is available in a range of dosage strengths, typically spanning from 10 mg to 80 mg.
The initial dosage is determined based on an individual's cholesterol levels, cardiovascular risk factors, and overall health.
Patients requiring more aggressive cholesterol reduction may be prescribed higher doses.
Atorvastatin is administered orally, usually once daily, and can be taken at any time of day, with or without food.
Consistency in timing is still recommended to maintain stable blood levels.
Efficacy: Clinical Evidence for LDL Cholesterol Reduction
Clinical trials have extensively demonstrated atorvastatin's effectiveness in lowering LDL cholesterol and reducing the risk of cardiovascular events.
Studies have shown that atorvastatin can significantly decrease LDL-C levels, often achieving substantial reductions even at moderate doses.
Furthermore, research has indicated that atorvastatin can improve other lipid parameters, such as triglycerides and HDL cholesterol, contributing to overall cardiovascular health.
The effectiveness of atorvastatin has been proven across a wide range of patient populations, solidifying its position as a reliable statin therapy.
Understanding the effects and function of rosuvastatin provides a basis for comparison. Next, we turn our attention to another widely used statin, atorvastatin, exploring its distinct characteristics and clinical profile.
Rosuvastatin vs. Atorvastatin: A Head-to-Head Comparison
Choosing between rosuvastatin and atorvastatin isn't a one-size-fits-all decision.
Both effectively lower cholesterol, but key differences impact which is more suitable for individual patients.
This section provides a direct comparison, examining efficacy, dosage, side effects, and patient-specific considerations to inform a more nuanced understanding.
Efficacy in Lowering LDL and Raising HDL Cholesterol
One of the primary considerations when choosing a statin is its ability to lower LDL ("bad") cholesterol and raise HDL ("good") cholesterol.
Rosuvastatin is generally considered more potent than atorvastatin at equivalent doses in lowering LDL-C.
Clinical trials have demonstrated that rosuvastatin can achieve greater LDL-C reductions, potentially making it a preferred choice for patients requiring aggressive cholesterol lowering.
However, both drugs effectively raise HDL-C, though the magnitude of increase can vary between individuals.
Dosage Considerations: Starting and Maximum Doses
Dosage is another crucial aspect of statin therapy.
Atorvastatin is typically initiated at doses ranging from 10 mg to 80 mg daily, while rosuvastatin usually starts at 5 mg to 40 mg daily.
While the maximum dosage for atorvastatin is 80 mg, rosuvastatin's maximum is 40 mg.
It's essential to note that higher doses don't always equate to better outcomes, and the optimal dose is determined by individual response and tolerability.
Side Effects: A Focus on Muscle Pain (Myalgia)
Like all medications, statins can cause side effects.
Muscle pain (myalgia) is among the most commonly reported side effects with both rosuvastatin and atorvastatin.
The incidence and severity of myalgia can vary among individuals, and it's not always predictable.
Some studies suggest a slightly higher risk of myalgia with atorvastatin, while others show no significant difference.
If you have experienced Statin intolerance in the past, or have certain existing muscular conditions, your doctor may consider prescribing a lower dosage, or a different Statin altogether.
Clinical Trials: Direct Comparisons of Rosuvastatin and Atorvastatin
Numerous clinical trials have directly compared rosuvastatin and atorvastatin.
These trials often evaluate their efficacy in reducing LDL-C, achieving target cholesterol levels, and preventing cardiovascular events.
Generally, these studies have confirmed rosuvastatin's greater potency in LDL-C reduction.
However, the choice between the two often depends on individual patient factors, tolerability, and specific treatment goals.
Patient-Specific Risk Factors and Health Conditions
Individual risk factors and co-existing health conditions significantly influence statin selection.
For example, patients with diabetes or kidney disease may require careful monitoring while on statins, and the choice of statin might be influenced by these considerations.
Rosuvastatin's greater potency may be advantageous for high-risk patients needing significant LDL-C reduction.
Ultimately, the decision should be made in consultation with a healthcare professional who can assess individual risk profiles and tailor treatment accordingly.
Choosing the Right Statin: Factors to Consider for Personalized Treatment
Having examined the distinct profiles of rosuvastatin and atorvastatin, the next crucial step lies in determining which statin is most appropriate for an individual. The selection process should never be arbitrary but rather a carefully considered decision based on a comprehensive assessment of various factors.
Individual CVD Risk Factors
An individual's overall risk of cardiovascular disease (CVD) is a primary determinant in statin selection.
This assessment typically involves evaluating several key risk factors:
-
Family History: A strong family history of premature heart disease significantly elevates an individual's risk, potentially necessitating more aggressive cholesterol management.
-
Age: Advancing age is an independent risk factor for CVD. Treatment strategies may differ for older versus younger patients.
-
Lifestyle: Lifestyle choices such as diet, exercise, and smoking habits profoundly impact CVD risk. These factors are considered alongside medication when managing risk.
Impact of Co-existing Health Conditions
The presence of other health conditions can significantly influence statin choice.
-
Diabetes: Diabetes is a major risk factor for CVD, and statin therapy is often a cornerstone of management.
- Certain statins might be preferred based on their impact on blood sugar control or potential interactions with diabetes medications.
-
Liver Function: Statins can, in rare cases, affect liver function.
-
Individuals with pre-existing liver conditions require careful monitoring and may need to avoid certain statins altogether.
-
Lower doses or alternative statins may be considered to minimize the risk of liver-related complications.
-
Drug Interactions and Polypharmacy
Many patients take multiple medications concurrently, a situation known as polypharmacy.
Drug interactions are a significant concern in these cases. Certain medications can interact with statins, either increasing the risk of side effects or reducing the statin's effectiveness.
-
It's crucial for healthcare providers to carefully review a patient's entire medication list before prescribing a statin.
-
Adjustments to dosages or alternative statins might be necessary to avoid potentially harmful interactions.
The Paramount Importance of Physician Consultation
While this article provides a comprehensive overview of rosuvastatin and atorvastatin, it is not a substitute for professional medical advice.
-
The "best" statin for any individual is a highly personalized decision that requires the expertise of a qualified healthcare provider.
-
A physician can assess a patient's unique risk factors, medical history, and medication profile to make an informed recommendation.
- They can also monitor the patient's response to treatment and adjust the dosage or medication as needed.
Ultimately, the goal of statin therapy is to reduce the risk of cardiovascular events and improve overall health. This requires a collaborative effort between the patient and their healthcare provider.
Safety and Side Effects: Navigating Potential Adverse Reactions with Statins
While statins like rosuvastatin and atorvastatin are generally well-tolerated and highly effective in reducing cardiovascular risk, it's crucial to be aware of potential side effects. Understanding these adverse reactions and how to manage them is essential for ensuring long-term adherence to statin therapy. This knowledge empowers patients and healthcare providers to make informed decisions and optimize treatment outcomes.
Common Side Effects of Rosuvastatin and Atorvastatin
Both rosuvastatin and atorvastatin share a similar side effect profile, with the most commonly reported adverse reactions being:
-
Muscle pain and weakness (myalgia): This is arguably the most frequent complaint among statin users. The severity can range from mild discomfort to debilitating pain.
-
Gastrointestinal issues: These include nausea, constipation, diarrhea, and abdominal discomfort.
-
Headache: Some individuals may experience headaches, particularly when starting statin therapy.
Less Common but Important Adverse Reactions
While less frequent, certain side effects require careful attention:
-
Elevated liver enzymes: Statins can, in rare cases, cause an elevation in liver enzymes, indicating potential liver inflammation or damage.
-
Increased blood sugar levels: Statins may slightly increase blood sugar levels, which is particularly relevant for individuals with diabetes or prediabetes.
-
Rhabdomyolysis: This is a rare but serious condition involving the breakdown of muscle tissue, which can lead to kidney damage. It is important to seek immediate medical attention if you experience unexplained muscle pain, tenderness, or weakness, especially if accompanied by fever, fatigue, or dark urine.
-
Cognitive issues: Some individuals have reported memory loss or confusion while taking statins.
Strategies for Managing Statin Side Effects
Fortunately, many statin-related side effects can be effectively managed:
Lifestyle Adjustments
-
Dietary changes: A heart-healthy diet low in saturated and trans fats can complement statin therapy and minimize gastrointestinal issues.
-
Regular exercise: While statins themselves can sometimes cause muscle pain, regular exercise can improve overall muscle health and potentially alleviate discomfort.
-
Hydration: Staying well-hydrated can help prevent muscle cramps and constipation.
Medication Adjustments
-
Lowering the statin dose: Reducing the dose can sometimes alleviate side effects without significantly compromising cholesterol-lowering efficacy.
-
Switching statins: If one statin causes intolerable side effects, switching to another statin (e.g., from atorvastatin to rosuvastatin, or vice versa) might be a viable option. Because each statin has a slightly different pharmacological profile, some individuals may tolerate one statin better than another.
-
Intermittent dosing: Some doctors may consider less frequent dosing schedules in some situations.
-
Adding Coenzyme Q10 (CoQ10): Some studies suggest that CoQ10 supplementation may help reduce muscle pain associated with statin use.
-
Non-statin therapies: In certain cases, alternative cholesterol-lowering medications (e.g., ezetimibe, PCSK9 inhibitors) may be considered, either alone or in combination with a low-dose statin.
The Importance of Liver Function Monitoring
Because statins can potentially affect liver function, regular liver function tests (LFTs) are typically recommended, especially when starting statin therapy and periodically thereafter. This allows healthcare providers to monitor for any signs of liver inflammation or damage and adjust treatment accordingly. Individuals with pre-existing liver conditions require particularly close monitoring.
A Proactive Approach to Safety
Being informed about the potential side effects of statins empowers patients to proactively manage their health. Open communication with your healthcare provider is crucial. Report any unusual symptoms or concerns promptly. Do not discontinue statin therapy without consulting your doctor, as abruptly stopping statins can increase your risk of cardiovascular events. Working collaboratively with your healthcare team ensures that statin therapy is both safe and effective in achieving your cardiovascular health goals.
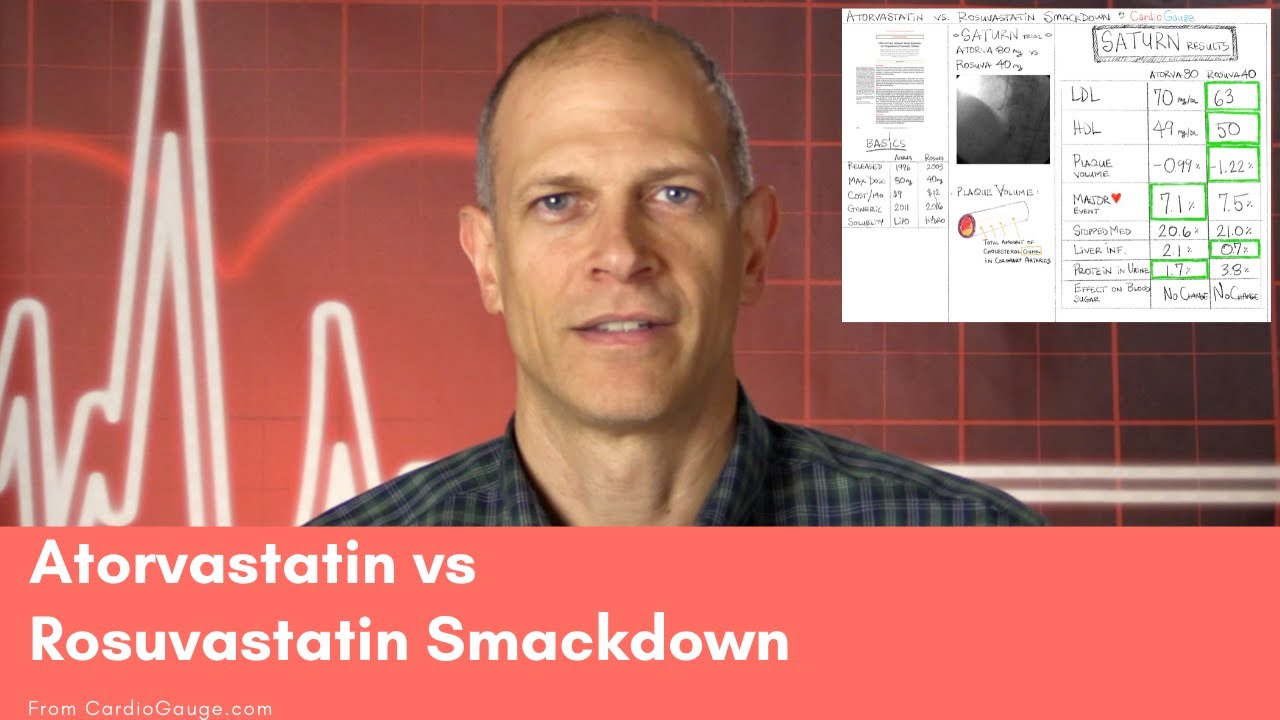
Video: Rosuvastatin vs Atorvastatin: Which Is Best For You?
FAQs: Rosuvastatin vs. Atorvastatin
Here are some frequently asked questions to help you understand the differences between rosuvastatin and atorvastatin.
Are rosuvastatin and atorvastatin the same thing?
No, rosuvastatin and atorvastatin are not the same. Both are statin medications used to lower cholesterol, but they have different strengths and potential side effects. Your doctor will decide which is best for you based on your individual health profile.
Which is more potent, rosuvastatin or atorvastatin?
Generally, rosuvastatin is considered more potent than atorvastatin. This means a lower dose of rosuvastatin may achieve the same cholesterol-lowering effect as a higher dose of atorvastatin. However, effectiveness can vary among individuals.
Are the side effects different for rosuvastatin vs atorvastatin?
The potential side effects are similar for both rosuvastatin and atorvastatin, including muscle pain, liver problems, and increased blood sugar levels. However, individual experiences may vary. Talk to your doctor about any concerns regarding side effects.
How do I know if rosuvastatin or atorvastatin is right for me?
The best statin for you depends on several factors, including your cholesterol levels, other health conditions, potential drug interactions, and your doctor's assessment. A discussion with your doctor is essential to determine if rosuvastatin or atorvastatin is the appropriate choice to manage your cholesterol.