BVM Ventilation: The Ultimate Guide to Saving Lives Now!
Effective BVM ventilation, often employed by first responders at Emergency Medical Services (EMS) scenes, remains a cornerstone of respiratory support in critical situations. The success of this manual ventilation technique heavily relies on adherence to established guidelines, often championed by organizations like the American Heart Association (AHA). Mastery of proper hand placement and ventilation rates, elements emphasized by pioneers like Peter Safar in airway management, is crucial for delivering adequate tidal volume and minimizing complications. This guide delves deep into the essential principles of bvm ventilation, equipping healthcare professionals and first responders with the knowledge to make a life-saving difference.

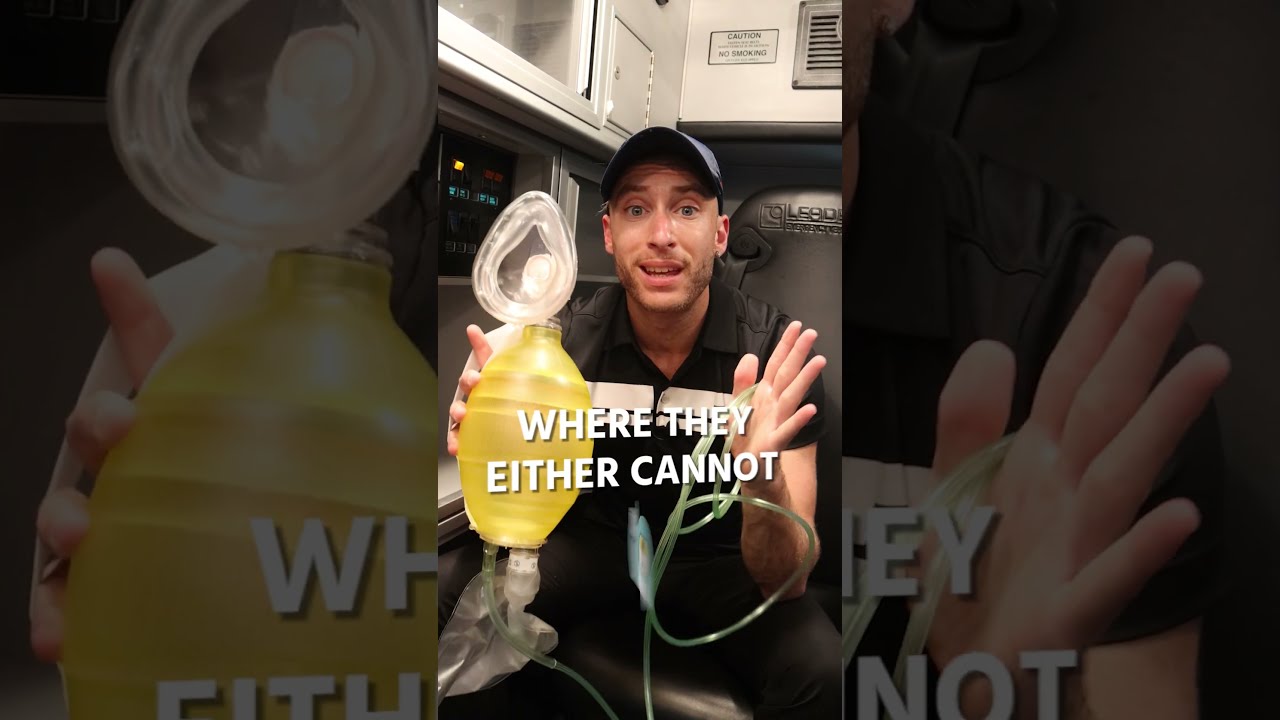
Image taken from the YouTube channel EMTprep , from the video titled EMT Skills: Bag-Valve-Mask (BVM) Ventilation - EMTprep.com .
Imagine a scene: a bystander collapses, unresponsive. Every second counts. The rapid response of trained individuals armed with a Bag-Valve-Mask (BVM) can be the critical difference between life and death. This highlights the urgency and sheer importance of effective BVM ventilation.
The ability to deliver manual breaths effectively using a BVM is a cornerstone skill in emergency medical care. It buys precious time, maintains oxygenation, and supports vital organ function until definitive care can be administered.
The Breath of Life: A Critical Intervention
BVM ventilation is more than just a technique; it's a vital intervention. It bridges the gap when a patient's own respiratory system falters. The BVM stands as a readily available, manually operated ventilator, capable of delivering life-sustaining breaths in countless scenarios.
Consider the implications of a sudden cardiac arrest, a severe asthma attack, or a traumatic injury compromising breathing. In each of these situations, the BVM becomes the primary means of providing necessary oxygen. It prevents hypoxia, and supports cellular function until the underlying condition is addressed.
BVM Ventilation: A Crucial Skill
Effective BVM ventilation is a crucial skill for healthcare providers and first responders. It demands both knowledge and proficiency. Mastery requires understanding the device. Skillful application ensures successful outcomes.
The urgency of emergency situations necessitates that professionals act quickly. They must be adept at using the BVM to maintain adequate oxygenation and ventilation.
This skill isn't merely an optional add-on. It is an essential element of emergency preparedness. It dramatically improves the odds of survival and positive patient outcomes.
Navigating the Essentials of BVM Ventilation
This discussion will guide you through the core aspects of BVM ventilation. The goal is to provide a comprehensive understanding. This includes understanding the BVM device and mastering proper techniques. It also covers advanced considerations for optimizing its effectiveness.
We'll explore the components of the BVM, step-by-step techniques for achieving effective ventilation. We'll cover application in specific emergency situations. We will also address troubleshooting strategies. This enables confident responses to challenges.
Imagine the comfort that comes from knowing that you can provide effective BVM ventilation to a patient in need. This ability stems from a strong understanding of the foundational principles. It is built on a solid grasp of what BVM ventilation is, its components, and the underlying physiological reasons for its use.
Understanding the Basics: What is BVM Ventilation?
At its core, BVM ventilation is a temporary method. It assists or replaces a patient's spontaneous breathing. It provides manual breaths using a Bag-Valve-Mask (BVM) device. This intervention delivers oxygen to the lungs. It removes carbon dioxide from the body.
It's a crucial skill that can be life-saving. It provides essential support. It bridges the gap until the patient can breathe independently or receive more advanced respiratory support.
Defining BVM Ventilation: The Act of Manual Respiration
BVM ventilation, also known as manual ventilation or "bagging," is the act of delivering breaths to a patient using a handheld device. This becomes essential when a patient is unable to breathe adequately on their own. This may be due to:
- Respiratory arrest
- Respiratory failure
- Depressed level of consciousness
- Neuromuscular disorders
- Other conditions affecting breathing
The process involves placing a mask over the patient's nose and mouth. A trained provider then squeezes the bag. This forces air (often enriched with supplemental oxygen) into the patient’s lungs. The goal is to maintain adequate oxygenation and ventilation until the underlying cause of the respiratory compromise can be addressed.
The Components of a BVM: A Closer Look
The BVM device consists of three primary components, each playing a vital role in effective ventilation:
- The Bag: This self-inflating bag is squeezed by the provider to deliver air into the patient’s lungs. Bag sizes vary. They are chosen based on the patient's age and size. Selecting the correct bag ensures appropriate tidal volume delivery.
- The Mask (Ambu Bag): The mask creates a seal over the patient’s nose and mouth, allowing for effective delivery of air without leakage. Masks come in various sizes to accommodate different patient demographics. Proper mask fit is critical. It ensures that air enters the patient’s lungs rather than escaping around the mask's edges.
- The Valve System: This system includes a one-way valve that directs airflow from the bag to the patient during inspiration. It prevents exhaled air from re-entering the bag. Some BVMs also include a positive end-expiratory pressure (PEEP) valve. It maintains pressure in the lungs at the end of exhalation.
Each component is vital for effective BVM ventilation. Understanding them is crucial for successful operation.
Why Ventilation is Crucial: The Physiological Imperative
Ventilation is one of the two facets of respiration. It is the mechanical process of moving air into and out of the lungs. It facilitates gas exchange. Oxygen moves from the inhaled air into the bloodstream. Carbon dioxide, a waste product of metabolism, moves from the blood into the lungs to be exhaled.
Adequate ventilation is essential for maintaining cellular function and overall survival. When ventilation is compromised, several detrimental consequences can arise:
- Hypoxia: Insufficient oxygen supply to the body's tissues and organs. This can lead to cellular damage, organ dysfunction, and death.
- Hypercapnia: Elevated levels of carbon dioxide in the blood. This can cause acidemia (increased acidity of the blood) and further compromise organ function.
- Respiratory Acidosis: A condition where the blood becomes too acidic due to the accumulation of carbon dioxide. This can impair enzyme function and disrupt cellular processes.
BVM ventilation counteracts these effects. It provides assisted or controlled respiration. This restores proper gas exchange. It maintains oxygen delivery. It prevents the buildup of carbon dioxide. In essence, it bridges the gap until the patient's natural respiratory function can be restored.
Imagine the comfort that comes from knowing that you can provide effective BVM ventilation to a patient in need. This ability stems from a strong understanding of the foundational principles. It is built on a solid grasp of what BVM ventilation is, its components, and the underlying physiological reasons for its use.
However, knowledge alone isn't enough. Truly mastering BVM ventilation requires a mastery of the practical techniques involved. Let’s break down the crucial steps to ensure you can confidently and effectively deliver this life-saving intervention.
Mastering the Technique: A Step-by-Step Guide to Effective BVM Ventilation
Effective BVM ventilation is not just about squeezing a bag; it’s a carefully orchestrated series of actions. Each step, from preparation to patient monitoring, contributes to successful oxygenation and ventilation. A methodical approach ensures the best possible outcome for the patient.
Preparing for Ventilation: Setting the Stage for Success
Before you even touch the BVM, take a moment to ensure your safety and preparedness. Scene safety is paramount. Assess the environment for any hazards and eliminate them if possible.
Next, don your personal protective equipment (PPE). Gloves, mask, and eye protection are essential to protect yourself from potentially infectious materials.
Finally, assemble the BVM. Ensure all components are present, intact, and connected properly. This includes confirming the reservoir bag is correctly attached to provide optimal oxygen delivery. A malfunctioning device is useless in an emergency.
Airway Management: Ensuring a Clear Path
A patent airway is the foundation of successful ventilation. If the airway is blocked, air cannot reach the lungs, rendering BVM ventilation ineffective.
Begin by using manual maneuvers to open the airway. The head-tilt/chin-lift maneuver is typically the first choice. However, if a spinal injury is suspected, the jaw-thrust maneuver is preferred to avoid further neck movement.
Consider adjuncts. Oropharyngeal airways (OPAs) and nasopharyngeal airways (NPAs) can help maintain airway patency. Select the appropriate size and insert them carefully to avoid complications.
Mask Seal: Creating a Leak-Proof Interface
Achieving a proper mask seal is critical. A leak-proof seal ensures that the air you deliver goes into the patient’s lungs and not into the surrounding atmosphere.
Use the “EC clamp” technique. Place the mask on the patient's face. Use your thumb and index finger to form a "C" shape, pressing down on the mask to create a seal. Use your remaining fingers to lift the jaw ("E" shape), bringing the patient's face to the mask.
Ensure the mask covers both the nose and mouth. Adjust the position as needed to minimize leaks. Beards or facial hair can interfere with the seal, so consider lubrication or other strategies to improve contact.
Providing Breaths: Delivering Effective Ventilation
With a patent airway and a good mask seal established, it’s time to deliver breaths. Squeeze the bag smoothly and consistently. Avoid rapid, forceful compressions, which can cause gastric distention or lung injury.
The appropriate rate and volume are crucial. Aim for a rate of 10-12 breaths per minute for adults. Each breath should be delivered over approximately 1 second. Observe for adequate chest rise as an indicator of sufficient volume.
Avoid over-ventilation. Excessive volume or pressure can cause barotrauma or other complications. Less is often more.
Monitoring the Patient: Assessing Ventilation Effectiveness
Continuous monitoring is essential to assess the effectiveness of your ventilation efforts. Look for chest rise. Adequate chest rise indicates that air is entering the lungs.
Listen for breath sounds. Auscultate both sides of the chest to ensure equal and adequate air entry. Absent or diminished breath sounds may indicate airway obstruction or other problems.
Monitor vital signs. Track the patient’s heart rate, blood pressure, and oxygen saturation. Improvements in these parameters suggest effective ventilation. Use capnography if available to assess exhaled carbon dioxide levels, providing valuable feedback on ventilation effectiveness.
BVM Ventilation in Emergency Situations: When to Use It
Having established a foundation in BVM ventilation techniques, it's vital to understand when and where this intervention becomes crucial. BVM ventilation serves as a critical bridge, maintaining oxygenation and ventilation in a myriad of emergency scenarios, until more definitive airway management or spontaneous breathing resumes. Its versatility makes it an indispensable tool across various healthcare settings.
Respiratory Failure
Respiratory failure signifies the lungs' inability to adequately oxygenate the blood or eliminate carbon dioxide. This can stem from diverse causes, including:
-
Pneumonia and other infections: Conditions where the lungs become inflamed and filled with fluid, impairing gas exchange.
-
Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease obstructing airflow.
-
Drug Overdose: Substances that depress the respiratory center in the brain.
-
Neuromuscular Disorders: Diseases like Muscular Dystrophy or Amyotrophic Lateral Sclerosis (ALS) that weaken respiratory muscles.
In these instances, BVM ventilation provides essential support by manually delivering breaths, ensuring oxygen reaches the bloodstream and carbon dioxide is removed. This buys crucial time for underlying conditions to be treated.
BVM Ventilation During CPR
Cardiopulmonary Resuscitation (CPR) aims to restore circulation and breathing in individuals experiencing cardiac arrest. The American Heart Association (AHA) guidelines emphasize the importance of early and effective ventilation during CPR. BVM ventilation is a cornerstone of this effort, providing the necessary breaths when a patient is unable to breathe independently.
AHA guidelines typically recommend a compression-to-ventilation ratio of 30:2 for adults when a single rescuer is present. This ratio shifts to 15:2 when two rescuers are available for children and infants (excluding newborns). Proper BVM technique is essential during CPR to avoid complications such as gastric distention or inadequate chest rise.
BVM Ventilation in EMS Settings
Emergency Medical Services (EMS) personnel frequently encounter situations demanding immediate respiratory support in pre-hospital environments. From traffic accidents to medical emergencies at home, EMS providers rely on BVM ventilation to stabilize patients en route to the hospital.
The portability and ease of use of the BVM make it invaluable in these dynamic settings. EMS providers use it to manage a wide range of conditions, including:
-
Traumatic Injuries: Chest trauma, head injuries affecting respiratory drive.
-
Asthma Exacerbations: Severe asthma attacks causing airway constriction.
-
Drowning: Providing immediate ventilation after water rescue.
BVM Ventilation During Resuscitation
Resuscitation efforts, whether in the hospital or pre-hospital setting, frequently require assisted ventilation. BVM ventilation is a primary method for delivering breaths during these critical moments. It is used in conjunction with other resuscitation measures, such as chest compressions and medication administration, to maximize the chances of a successful outcome.
The decision to initiate BVM ventilation during resuscitation depends on factors such as:
-
The patient's level of consciousness: Unresponsive patients typically require ventilation.
-
Respiratory rate and effort: Labored or absent breathing necessitates intervention.
-
Oxygen saturation levels: Low oxygen saturation despite supplemental oxygen indicates the need for assisted ventilation.
Having established the foundational techniques and appropriate scenarios for BVM ventilation, it's crucial to explore the advanced strategies that can significantly enhance its effectiveness. Maximizing oxygen delivery, optimizing the procedure with multiple rescuers, and adapting the technique to suit diverse patient needs are all essential components of expert-level BVM ventilation. These considerations can make a critical difference in patient outcomes, particularly in complex or challenging situations.
Optimizing BVM Ventilation: Advanced Considerations
While basic BVM ventilation can be lifesaving, mastering advanced techniques elevates the standard of care. These considerations – from enriching oxygen delivery to employing two-rescuer techniques and adapting to special populations – are essential for maximizing the effectiveness of BVM ventilation.
The Power of Supplemental Oxygen
Ambient air contains approximately 21% oxygen. In emergency situations, this may be insufficient to meet the patient's needs. Supplementing BVM ventilation with oxygen significantly increases the fraction of inspired oxygen (FiO2), potentially reaching close to 100% when delivered properly.
This is particularly crucial in cases of severe respiratory distress or cardiac arrest.
Delivery Methods for Supplemental Oxygen
Oxygen can be delivered to the BVM via several methods:
-
Oxygen Reservoir: Many BVMs have an oxygen reservoir bag attached. When connected to an oxygen source, this reservoir fills with oxygen, providing a higher FiO2 during ventilation.
-
Direct Connection: Some BVMs allow for direct connection to an oxygen source, delivering a continuous flow of oxygen into the bag.
Titration and Monitoring
It's important to remember that oxygen is a medication and should be titrated to the patient's needs.
Ideally, pulse oximetry should be used to monitor the patient's oxygen saturation (SpO2). The goal is to maintain an SpO2 within the target range (typically 94-98% for most patients).
Two Hands Are Better Than One: The Two-Rescuer Technique
Achieving an effective mask seal is paramount for successful BVM ventilation. A poor seal results in air leakage, reducing the amount of oxygen delivered to the patient's lungs.
The two-rescuer technique is a game-changer, significantly improving mask seal and overall ventilation efficacy.
Roles and Responsibilities
In the two-rescuer technique, one rescuer focuses solely on maintaining a tight mask seal. This rescuer uses both hands to secure the mask to the patient's face, using the "EC clamp" technique.
The other rescuer is responsible for squeezing the bag, delivering breaths at the appropriate rate and volume.
Advantages of the Two-Rescuer Approach
-
Superior Mask Seal: The primary benefit is the improved mask seal, minimizing air leakage and maximizing oxygen delivery.
-
Reduced Fatigue: Sharing the workload reduces rescuer fatigue, allowing for more consistent and effective ventilation over extended periods.
-
Improved Coordination: With clearly defined roles, the two-rescuer technique promotes better coordination and communication, leading to more efficient ventilation.
Adapting to Special Populations
While the fundamental principles of BVM ventilation remain consistent, certain patient populations require special considerations. Infants, children, and individuals with facial trauma present unique challenges that necessitate adjustments to technique and equipment.
Infants and Children
-
Smaller Tidal Volumes: Infants and children require smaller tidal volumes than adults. Excessive ventilation can lead to barotrauma (lung injury).
-
Appropriate Mask Size: Using a mask that is appropriately sized for the patient's face is crucial for achieving a proper seal. Infant and child-sized masks are essential.
-
Higher Respiratory Rates: Infants and children typically have higher normal respiratory rates than adults. Adjust the ventilation rate accordingly.
Patients with Facial Trauma
Facial trauma can make it difficult to achieve an adequate mask seal.
-
Alternative Techniques: Consider using alternative airway management techniques, such as a supraglottic airway device, if BVM ventilation is ineffective due to facial trauma.
-
Gentle Ventilation: Apply gentle pressure when ventilating patients with facial trauma to avoid exacerbating injuries.
Troubleshooting Common BVM Ventilation Problems
Even with proper training and technique, challenges can arise during BVM ventilation. Recognizing and addressing these issues promptly is paramount to ensuring effective oxygenation and positive patient outcomes. This section will explore common problems encountered during BVM ventilation and provide practical solutions for overcoming them.
Addressing Inadequate Chest Rise
One of the most immediate indicators of effective ventilation is visible chest rise. If the chest isn't rising adequately with each breath delivered, it signals a problem that demands immediate attention. Several factors could be at play, each requiring a specific approach.
Poor Mask Seal
A poor mask seal is a frequent culprit. Air leaking around the mask prevents sufficient pressure from reaching the lungs. Reassess the mask position, ensuring it covers the mouth and nose completely. Utilize the "EC clamp" technique, using one hand to hold the mask firmly against the face while the other hand squeezes the bag. Consider using two rescuers, one dedicated to maintaining the mask seal while the other delivers breaths.
Airway Obstruction
An obstructed airway hinders the flow of air to the lungs. Common causes include the tongue falling back, foreign objects, or secretions. Employ airway maneuvers such as the head-tilt/chin-lift (unless contraindicated by suspected spinal injury) or the jaw-thrust maneuver to open the airway. Suctioning may be necessary to remove any obstructing fluids or debris. If these measures prove insufficient, consider advanced airway techniques, if appropriately trained and authorized.
Inadequate Tidal Volume
Insufficient squeeze of the bag results in inadequate tidal volume. Ensure you are delivering enough air with each breath. Observe the chest rise carefully and adjust the squeeze accordingly. Remember that excessive volumes can be harmful, so aim for visible chest rise without over-inflation.
Minimizing Gastric Distention
Gastric distention, the inflation of the stomach with air, is a potential complication of BVM ventilation. It can lead to vomiting, aspiration, and reduced lung capacity. Several techniques can help minimize this risk.
Avoid excessive ventilation pressure and rate. High pressures force air into the esophagus rather than the trachea. Deliver breaths slowly and gently, aiming for just enough volume to achieve chest rise.
Ensure a patent airway. An obstructed airway increases the likelihood of air entering the esophagus. Prioritize airway management techniques as described above.
Consider applying cricoid pressure (Sellick maneuver). This involves applying pressure to the cricoid cartilage to compress the esophagus, potentially reducing the risk of air entering the stomach. However, the routine use of cricoid pressure is debated, and its effectiveness is not definitively proven in all situations.
Recognizing and Responding to Complications
While BVM ventilation is a lifesaving intervention, it's essential to be aware of potential complications and how to manage them.
Aspiration is a risk if the patient vomits. Be prepared to suction the airway immediately if vomiting occurs. Position the patient on their side, if possible, to facilitate drainage.
Pneumothorax (collapsed lung) can occur, especially with excessive ventilation pressures. Be vigilant for signs of pneumothorax, such as sudden respiratory distress, unequal chest rise, or absent breath sounds on one side.
Hypotension (low blood pressure) can be exacerbated by positive pressure ventilation. Monitor blood pressure closely and be prepared to provide fluid resuscitation if needed.
Hyperventilation leads to reduced CO2 levels. It's crucial to maintain the appropriate ventilation rate of around 10-12 breaths per minute. If recognized, reduce the rate and depth of ventilation.
By anticipating and addressing these common challenges, healthcare providers and first responders can significantly improve the effectiveness of BVM ventilation and ultimately enhance patient outcomes in critical situations.
Maintaining Competency: The Importance of Training and Practice
Effective BVM ventilation isn't a skill mastered once and then forgotten. It demands consistent effort and a commitment to maintaining proficiency. The infrequent nature of its use in real-world scenarios makes regular training and practice absolutely essential. This section will explore why ongoing education and skills maintenance are critical for healthcare professionals and first responders.
The Imperative of Regular Practice
Skills decay is a real phenomenon, especially with infrequently used procedures. BVM ventilation, while fundamental, falls into this category for many practitioners. To combat this, regular, hands-on practice is indispensable.
This doesn't necessarily require elaborate simulations every time. Short, focused drills can be highly effective. These can include:
- Practicing mask seal techniques.
- Refining bag-squeezing rhythm and volume.
- Running through different airway management scenarios.
These drills help to reinforce muscle memory and decision-making skills, ensuring that when a real emergency arises, the response is instinctive and effective. Furthermore, incorporating realistic scenarios during training—such as simulated patient deterioration—can better prepare individuals for the stress and complexity of actual emergencies.
Adhering to AHA Guidelines: A Foundation for Excellence
The American Heart Association (AHA) guidelines represent the gold standard for CPR and emergency cardiovascular care. These guidelines are based on the latest scientific evidence and provide a framework for best practices.
Following these guidelines is crucial for several reasons:
- Standardization: AHA guidelines promote consistent care across different settings and providers.
- Evidence-Based Practice: They ensure that BVM ventilation techniques are grounded in the most up-to-date research.
- Improved Outcomes: Adhering to these guidelines is linked to better patient outcomes in emergency situations.
Regular review and application of AHA guidelines is crucial. This includes understanding the recommended ventilation rates, tidal volumes, and the integration of BVM ventilation within the broader context of resuscitation efforts.
The Necessity of Continuous Education
The field of emergency medicine is constantly evolving. New research, technologies, and techniques emerge regularly. Continuous education is therefore vital for healthcare providers and first responders to stay abreast of these advancements.
This education can take many forms:
- Attending conferences and workshops.
- Participating in online courses and webinars.
- Reviewing professional journals and publications.
Staying informed about the latest advancements in BVM ventilation ensures that practitioners are equipped with the most effective and up-to-date knowledge and skills. For example, understanding the nuances of ventilation strategies in patients with specific conditions, like acute respiratory distress syndrome (ARDS), can significantly impact patient outcomes. This understanding only comes through ongoing learning and professional development.
Video: BVM Ventilation: The Ultimate Guide to Saving Lives Now!
Frequently Asked Questions About BVM Ventilation
This FAQ section addresses common questions related to bag-valve-mask (BVM) ventilation, as discussed in "BVM Ventilation: The Ultimate Guide to Saving Lives Now!". We aim to clarify important points and provide quick answers to enhance your understanding of this life-saving technique.
Why is proper mask seal so crucial during BVM ventilation?
A tight mask seal is essential for effective bvm ventilation. Without it, air leaks occur, preventing adequate oxygen delivery to the patient's lungs. A poor seal significantly reduces ventilation effectiveness, potentially leading to hypoxia.
What if I'm having trouble maintaining an open airway during BVM ventilation?
Maintaining an open airway is paramount. Use maneuvers like the head-tilt/chin-lift or jaw-thrust (especially if spinal injury is suspected). Consider using adjuncts like an oropharyngeal (OPA) or nasopharyngeal airway (NPA) to help keep the airway patent, ensuring effective bvm ventilation.
How do I know if I'm ventilating too quickly or forcefully with the BVM?
Look for chest rise. Excessive chest rise, gastric distention, and potential barotrauma (lung injury) can occur with over-ventilation. Aim for gentle, consistent ventilations – about 10-12 breaths per minute – while watching for adequate chest rise. This is crucial for avoiding complications associated with bvm ventilation.
What are some situations where BVM ventilation might not be enough, and I need to consider other options?
If bvm ventilation isn't effectively oxygenating the patient (as evidenced by poor SpO2 readings), or if the patient has significant airway obstruction, alternative advanced airway management techniques like endotracheal intubation or supraglottic airway devices might be necessary. Persistent difficulty with ventilation requires reassessment and escalation of care.